"Go With Us!" to EULAR 2024
AiArthritis Voices 360, Episode 101
Air Date: September 1 , 2024
This episode is a Step5, as outlined in our 6 Step Patient-Led Problem Solving Process.
In this episode, our co-hosts bring you an exclusive look into the AiArthritis “Go With Us!” to Conferences program. We dive deep into EULAR 2024, the European Rheumatology Research Conference, where patients and co-hosts reveal groundbreaking advancements in AiArthritis research. Discover the latest on CAR-T therapy, innovative pain management tailored for patients, the role of opioids in addressing pain and fatigue, and practical strategies for battling brain fog. Gain valuable insights and practical advice from fellow patients and experts. Don't miss this episode packed with cutting-edge information!
If you're eager for more, join us for our next journey to the ACR conference in November. Visit AiArthritis.org/conferences for more details and to sign up!
Episode Highlights:
- Overview of the Go With Us to Conferences program, which allows patients to virtually join and learn from major rheumatology conferences like EULAR and ACR.
- Tiffany, CEO and person living with non-radiographic axial spondyloarthritis, discusses CAR-T therapy and its potential to achieve remission in autoimmune diseases, particularly in lupus patients.
- Deb, AiArthritis volunteer and person living with rheumatoid arthritis, presents on patient-tailored pain management, emphasizing multi-dimensional approaches to address different types of pain.
- Becky, AiArthritis volunteer and person living with Sjogren’s Disease, explores the relationship between fatigue, pain, and opioids, highlighting the challenges of treating these symptoms in autoimmune patients.
- Leila, AiArthritis Health Education Manager and person living with Lupus Nephritis and Sjogren’s Disease, covers cognitive dysfunction (brain fog), offering strategies for managing this common but under-discussed symptom in autoimmune diseases.
AiArthritis Voices 360 is produced by the International Foundation for Autoimmune and Autoinflammatory Arthritis. Visit us on the web at
www.aiarthritis.org/talkshow. Find us on Twitter, Instagram, TikTok, or Facebook (@IFAiArthritis) or email us (podcast@aiarthritis.org). Be sure to check out our top-rated show on
Feedspot!
-
Expand to View the Podcast Transcript
[00:00:00] @Intro: Welcome to AiArthritis Voices 360, the podcast
solving today's most pressing issues in the AiArthritis community. We
invite you all to the table where together we face the daily challenges of
autoimmune and autoinflammatory arthritis. Join our fellow patient
cohosts as they lead discussions in the patient community, as well as
consult with stakeholders worldwide to solve the problems that matter
most, whether you are a loved one, a professional working in the field, or
a person diagnosed with an AiArthritis disease, this podcast is for you.
So pull up a chair and take a seat at the table.
[00:00:44] Tiffany: Hello, welcome to AiArthritis. Voice is 360. This is the
official talk show for the International Foundation for Autoimmune and
Autoinflammatory Arthritis, or AiArthritis for short.
My name is Tiffany Westridge Robertson. I am the CEO and original
founder of the organization. Also a person living with AiArthritis
diseases, primarily non-radiographic axial spondyloarthritis, and I am
very, very excited to bring to you this month's episode of our talk show,
which features one of our most popular programs we have at AiArthritis,
and that is our Go With Us to Conferences program.
In this case, it is EULAR 2024, the European Rheumatology Research
Conference. And EULAR is for the European Alliance of Associations for
Rheumatology. We are super, super, super excited to bring you some
highlights as this month's episode. As we do every year, twice a year, is
we go to the biggest scientific conferences of the year.
One is EULAR, and that happens in usually June of each year. And then
we also attend the American College of Rheumatology Convergence,
which is in November of each year. So stay tuned for ACR 2024 and
make sure you sign up to go with us virtually of course, can't take
everybody in person, but sign up virtually at AiArthritis.org/conferences.
So let me tell you a little bit about what go with us to conferences
program is all about. So that I can set you up to listen to some of the
clips or watch depending on how you're participating in our talk show
today. This is a program that was created by patients, including myself
and shout out to Deb Constine, who's you're going to hear from on this
episode because she was going with us as a person living with
rheumatology, rheumatoid arthritis.
My goodness, what's happening to my tongue today, rheumatoid
arthritis. And she is also a retired dietitian. And she's a co founder of this program. So she's been building this with me alongside in 2020. And
then since we brought on other staff, they have also been helping
develop and build this program.
So essentially the initial idea was we are going and learning all of this
amazing material this amazing information and we need to share it with
our community because it is not just about the research going on. The
information we're learning about treatments about health management,
disease management so relevant to our journeys. The issue is really,
these are conferences primarily with the audience being rheumatologist
and researchers now, at EULAR which is this one, it is a little unique
because they actually have a patient track at ACR they do not. But either
way, it is important we felt for patients to really understand and be able
to learn with us. And so we developed this program in order not just to
reiterate back what we're learning, but really have conversations, really
talk to each other, talk to you and help you understand how you can
relate this to communications with your doctors, to your own disease
management journey.
Because we do learn about pharmaceutical therapies and research and
different treatments, which you'll hear a snippet about today, but we also
learn about symptom control and you'll hear a little bit about brain fog
and fatigue. So those are the kind of things we're learning. And of
course, that's interesting, right?
And things that you want to learn as well. So this is, you're going to hear
today three of the debriefs that we did, or I'm sorry, four of the debriefs,
my goodness, that we did from EULAR 2024 from those patient leaders
who were going with us. So from myself, you will hear about CAR-T.
That is a new therapy that takes our own blood, our own metabolic
structure of our own bodies. We, we take the blood that goes into a lab,
it gets mixed up, it comes back and infused into your body and as a
result, you are healing yourself. It is a very novel process and it is
happening largely in the lupus community and also in a few other of our
diseases. So I will be doing a high level update on that, and then we'll
also have Deb reporting back to you on patient tailored pain
management.
Leila is going to be talking about what she learned about brain fog. And
then Becky is going to talk about the opioids and fatigue so she's going
to be talking about that. So you can see that there's quite a variety
again, you can learn more and sign up to go with us at AiArthritis.org/conferences and I'm going to turn it over to Ryan, our
producer to piece this together and let you witness some, a little taste of
what happens when you go with us to, in this case, EULAR 2024. First
up, we'll start with my debrief, which is on CAR-T. And here we go.
Hello, everybody. I'm excited to report on some sessions from EULAR
2024, specifically regarding precision medicine or the science of taking
our unique, signatures, molecular signatures from our blood, urine, and
zeroing in on things like genetics, DNA, et cetera.
And we've been focusing on this for a few years now at these
rheumatology conferences and how by doing so we can expedite
diagnosis. And we can also match treatments to people depending on
what might work better or worse for different subgroups. An
advancement, CAR-T, C A R dash T. You may have heard of it.
It's something that's been used in the cancer space for about a last
decade. And it has recently moved into the rheumatology space very
early. It's not something that you could get in your office, even close to
getting in there in the near future. But this is important and this is why we
go and we learn and we see what the potential is out there.
So this is very exciting. The CAR-T, which is essentially they go in, they
pull out, in this case, T cells. So T cells from your body, they put them
into a lab, they mix them all up with some other things, they put them
back in your body and then what ends up happening in the studies, we
had one lupus patient, then six lupus patients.
And what ended up happening is with that one dose, all went into
remission. And not just remission, like what we might think of as
remission, like low disease activity, like, no disease activity completely
off of all medications. And so that happened three years ago. We did
hear about it I think last year at one of the conferences and they gave us
an update and said, the person is still in remission and these were not
people with mild disease.
These are very serious. One needed a kidney transplant. So that just
shows you the power of these. It is a one and done we think, but we
don't know. That's also something important to understand with this
CAR-T therapy it of course can be very expensive. We have no idea. Is
it going to last five years? Is it going to last 10 years?
Is going to last 50 years? We don't know and that's part of what's
happening And the trials is trying to figure out as they follow these
patients who are at it so in saying that I wanted to give you let's see a
very specific i'm going to go into a patient with lupus and heart and lung
disease And treated with this CAR-T with this T cell extraction didn't
know if it was going to work, but they were, this person was so severe
they thought they would give it a try, even though they were completely
depleted of all of their B cells, which, cause they were on rituximab. And
that is one of the biologics that really do strip your immune system. But
even with that she grew all of the B cells back and replenished, went into
remission in 30 days, 100 percent remission, no medications.
So pretty amazing stuff, don't you think? I wanted to let you know too, it's
not just lupus, they're doing these CAR-T studies on myositis,
scleroderma, also known as systemic sclerosis. There's some debate
though. Who's going to get these when they are already, right? What is,
how refractory or refractory means not responding well to many
treatments, so you really are not responding to anything.
What's going to determine that? Who's going to get access to these? So
there is a really big debate there. The other part of that is what diseases,
so we have diseases like rheumatoid arthritis that are, for a lot of
patients can be treated pretty easily, but what about the rest of us?
Would we even be in line?
We don't have RA, but the point is who gets it? And so that's really just a
big discussion. And then to note, though, any existing damage, of
course, can't be repaired. If you have any type of, Things that have
happened because of your RA or because of your lupus or Sjogren's or
anything that cannot be undone but so you do have to consider that as
far as remission goes and then another session that I watched was
specific to Scleroderma or systemic scleritis, but I do want to point out
just because I'm saying that don't tune out.
Don't say oh Not my disease. I don't care. You do care. Let me tell you
what because these studies are make the rest, open the doors for the
rest of us. So understanding and being educated on the possibilities is
something that we all should talk about and learn about. It also ties into
when do we get treated?
So before they started talking about the CAR-T or the precision medicine
in diseases that don't have as many treatments don't have as many as some of the other diseases, they're having to really start to understand
when is the right time to treat. We do know historically. All of our
diseases, we have seen a, a process called treat to target, or working
with a rheumatologist to be on a drug after a certain amount of time not
working so well, we shift, we, and that is a treat to target.
We know that works. We have seen research presented to us in the last
several years, showing those who are treated early with the right
treatment have better outcomes actually can achieve a remission. It's it's
an actual word that we're actually seeing but it all it always involves that
early intervention.
So that is obviously something that they're targeting here but they also
need to understand is they're developing treatments and developing
treatments that are precise whether it's CAR-T or simply targeting
certain molecules or different signatures so that they can see what's
working best, they're going back to all of the old research for these
clinical trials for they specifically were doing ectemera.
So they looked through and they said, where are our subgroups?
Because back when these studies went on, they weren't considering
what might respond better in male, female, what might respond better in
a person who has long term disease versus early disease. And so all of
these are subgroups.
What subgroup do you fall into? So these are things that they went back
and they're looking and seeing, did any of these people in this group
respond better or worse? And they did find out that there were some
data that showed early intervention helped with the skin outcomes. And
it also did matter if they had never been treated before and they were
early on, they seemed to respond better to people who had been on
treatments and had the disease longer.
So that's interesting in itself because why did, why does it matter if
you've been on these treatments before versus not? So something
matters, but it's just part of what they're trying to explore and understand.
They also were looking for what they call predictive markers. So this is
something we've been working on in RA, Sjogren's.
Oh my gosh so much in Sjogren's. And I know we're reporting back on,
on that as well, but psoriatic arthritis, spondyloarthritis, there are these
predictive markers that they're starting to figure out. One biologic works better than others. And wow, wouldn't that be amazing if you could just
know, Hey, this is going to work for me.
So that is all in the process right now. And so they are starting to follow
patients in different trials to figure out these subgroups and who might
be responding better than others. Let me see. I'm looking at my notes
here. And there's another one and it did talk about the CAR-T specific in
these patients with scleroderma or systemic sclerosis, and it, they
treated seven patients.
So now we've got enough. These are small studies. So they're starting
very small and eventually they'll get bigger. And we had what a hundred
percent in the ones that I just reported back. In this one it was seven
patients during the three months after they received this infusion of the
CAR-T, the therapy, over 70% of these antibodies that were causing
their diseases dropped, and so they were able to see this improvement
in the skin disease and disease act activity overall just decreased about
30% after 120 days, and their ulcerations decreased within four weeks.
At 400 plus days, so over a year, everyone achieved significant
improvement. I want to point out, though, that they didn't talk about
remission and drug free in this one. I don't know what the difference is
between the lupus patients that had such success and the scleroderma
patients that didn't quite achieve remission.
There was also one patient that their levels kept going back up again, so
they didn't fully respond as well. So we, I don't know why, I don't know if
there was something else, a comorbidity or a multi diagnosis that, that
may have impacted that. I'm not sure they didn't go over that, but it
would be interesting to note.
So wrapping it up. It's just really good to know that all of this type of
research, it's early, but it's happening and they're stretching out to many
diseases and just curious, what are your thoughts about this exciting
new era of treatment? So we're really starting to think about this word
remission.
It's just amazing. So there's my report and more coming here from
EULAR 2024. All right, next up, let's turn it over to Deb Constein. As
mentioned, Deb is one of the co founders and co creators of this Go
With Us to Conferences program. She's a person living with rheumatoid
arthritis, a retired dietician, and a long term volunteer with AiArthritis.
Let's turn it over to Deb to talk about patient tailored pain management.
[00:15:58] Deb: Hi everybody. Deb Constein here, part of our core team
that is attending EULAR 2024. I'm in Madison, Wisconsin, longtime
volunteer of AiArthritis, and I have rheumatoid arthritis for the last 43
years, diagnosed at 13. The session I dug into today, and the reason I'm
looking down is I have lots of notes in front of me.
So just so you know why I'm not picking up all the time. The session I
chose was Patient Tailored Pain Management in RMDs. RMDs are
Rheumatological Musculoskeletal Diseases, are rheumatology type
diseases. And the professor that did this session was Professor Neil
Basu, B A S U, if I'm pronouncing that incorrectly.
He's the Professor of Musculoskeletal Disease in the University of
Glasgow. And one thing that he did focus on was he doesn't blame
patients for their number one priority being pain. So it was ranked pain,
fatigue, valued activities, low mood, mobility, activities of daily living, and
then visible joint damage.
And clearly I have visible joint damage. And this was consistent across
any rheumatological disease. And like psoriatic arthritis, lupus, all of
them are included. He did talk about the impacts of all aspects of patient
life being functional activities, social consequences, the economic
burden, and emotional well being.
So those are all the things that impact patients on a daily basis. And as
we've all seen that they call it the visual VAS. It is the 1 through 10 pain
number system. And it's got like from zero pain and you've got a smiley
face and at 10, they have tears and crying and things like that. He said,
that is not the way we should be looking at pain at this point.
We should be looking at it as an entire multi dimensional disease and
problem. And he talked about mapping out the different areas of the
brain that are affected by pain as well. He delved deep into three areas
of the mechanism descriptors of pain. The number one was nociceptive.
Now that is pain that arises from actual damage or something that
causes tissue issues, and it is like an example of that would be
inflammation in the joint or a broken bone for that matter.
The second one was neuropathic. That is pain that is caused by the
somatic sensory nervous system, and I know I said that kind of butchered a bit, but what that is actually talking about is part of our
sensory system that causes perception of touch, pressure, pain,
temperature, things like that so you understand what that is talking
about.
And that, an example of that would be like vasculitis. It's a, it's a
neuropathic pain disorder. RA would be a nociceptive so that number
one, that was an example of that as well so that inflammation in the joint.
And then the third piece, which he spent a lot of time on, was the
nociplastic, and that is pain that happens from an altered, there's no
clear evidence of there actually is an issue, and I could say that I have a
nociplastic pain sensation right here, but you can see that there's
nothing there.
There's no bruise. There's no evidence of the of a trauma or something
like that and things that they threw into this category was fibromalacia as
well as hypermobility things like that, there's no clear evidence and when
they talked about what to do about this third area, which is the
nociplastic pain, they recommended going to the EULAR
recommendations and you do a lot of education and exercise those
pieces that they thought that tended to have a really good influence on
people's pain in their body. And they also talked about the importance to
treat the symptoms that are related to pain. And so the fatigue, the
anxiety, the depression, all of those things too. They talked about those
can be equally as important as the pain that you're feeling and they said
when the exercise and education, when that is not enough, that you
need to actually start looking at treating all of the things that are
happening alongside of the pain. For some people, they can do it in a
pharmacological way. If you're having sleep disturbances or anxiety,
there's medications you can take. But they talked about the non
pharmacological management. And looking at basically a constant
behavioral therapy, so people talking to you, and that can be even over
the phone talking to a counselor, but that being all the time, as well as
exercise therapy, that can actually be also done, as well as visual care is
what they interpreted into being more the educational that happens.
And let's see, so they a couple other things that I wanted to quickly talk
about was they actually talked about visual, the functional MRI brain
imaging so it can actually look at the oxygenated and deoxygenated
Hemoglobin, so the blood in your brain, and measure it as far as the
activity goes and what's happening.
And, they're actually experimenting. Nothing is out there right now. But
they're really doing some, some research into the functional brain
imaging. And, looking at very specific of the brain. And, looking at that,
they think that certain areas of the brain are talking to each other. And
they're looking at the focus on that.
So there was something called at the very end, it was called the TMS.
It's a magnetic image, like a magnetic treatment. So a, a something like
a tool was put on the brain and it is called transcranial modulation and
it's using magnets and trying to target certain parts of the brain to use a
significant magnetic impulse to that specific part of your brain and they're
seeing that is having really good observation on the outcome of pain.
Really interesting study and there's more to come because they say that
this is an ongoing thing and we need to make sure we're really driving it
because it's the number one priority for patients as most of us
understand that for sure. So stay tuned, more to come.
[00:24:20] Tiffany: Okay, that was awesome, right? Next up, we have
Becky or Rebecca.
We've been calling her Becky. So Rebecca Hosey and Rebecca is a
health care professional, also a person living with Sjogren's disease.
And this was her first time going with us. So way to go, Becky. And this
is a highlight of her report on opioids, pain, and fatigue. So take it away.
[00:24:50] Becky: Hi everyone, Becky Hosey here again reporting on
some really cool things I learned.
The session that I watched was on fatigue, pain, and opioids, and
actually I'm going to break it up into two videos because all the
information is so important, but I don't want to overwhelm you. Just did
one long one, so I'll either record another video today or tomorrow.
Really as soon as I saw this title of the session, I knew I had to watch it.
So pain and fatigue are seriously underappreciated in our patient
population. And I also have an interest because I have over 10 years of
clinical experience working in interventional pain medicine, so I have a
bit of knowledge on this as well. The first presenter was so fascinating.
She's a rheumatologist, and she started the talk by saying how many
times her patients have reported to her that the fatigue and pain are
worse than, say, like, joint swelling or other symptoms.
And she also noted how these needs are largely unmet in our patient
population. A study in the U. S. on RA noted that the most impactful
symptoms were fatigue at 82% and pain at 76%, and sadly, in this study,
only 26% of these patients were actually satisfied with their RA
treatment.
Multiple studies suggest that fatigue is actually the number one and pain
number two most disabling symptoms regardless of whether the
condition is inflammatory or non inflammatory. So that was quite
interesting. The presenter went on to explain why fatigue and pain are
so underappreciated. And really it's that providers can, they can't see
fatigue or pain, right?
So they can see like joint deformities and they can see swollen fingers
and toes and everything, but they can't see fatigue or pain. And she also
noted, she thinks there's a lot of under reporting by patients. So patients
are not telling their providers about the symptoms either because they
don't think the provider will understand, or maybe they just think, Oh, it's
part of this disease, or they have difficulty explaining the symptoms.
Another issue that she discussed was that there's no really clear
consensus of a definition of fatigue in medicine. It's really subjective.
And it's really complicated and it has various subtypes. And she talked
about two main categories, physical fatigue and psychological fatigue,
right? So we know the physical fatigue, this low energy, this muscle
weakness, which she described as jelly legs and psychological fatigue,
the brain fog, the cognitive things, the weariness.
And of course, these types can occur together. They can occur in
combination at the same time or come back, leave, return another day,
all types of things. Interestingly, the idea of better controlling the disease
and the fatigue will get better has actually not been shown in clinical
studies. Multiple studies show the opposite.
So one in particular was a presentation that showed over 60 percent of
patients with RA, psoriatic arthritis, and spondyloarthritis who reported
fatigue even though they had really low disease activity. So their disease
was really well controlled. They still reported fatigue. So switching gears
to pain, there are accepted definitions of pain, but it's certainly not
uncomplicated.
But pain is really an unpleasant sensory and emotional experience and
this is a personalized experience, right? It's influenced by our biology,
our psychology, social factors, things that have happened to us. And
studies show that pain doesn't always equal inflammation. And studies
with patients with RMDs who complain of pain, even when in remission,
show that they still have residual pain, even though there's, the
inflammation is low and there's optimal treatment.
One presenter said that while medicine has done a really good job of
blocking pathways for inflammation, coming up with medications for
these, there really has been a poor, a poor outcome for studying and
treating pain. The three main pain categories, nociceptive pain, which
arises from actual or threatened tissue damage.
So these are of non nerve tissues and the activation of nociceptors. And
one, one presenter was in, she said, this is pain as it should be, an
alarm telling you there's something wrong. And examples of this are
tissue damage, joint inflammation. Neuropathic pain arises due to
nerves being affected and a lot of times, and not all the time, but it can
follow a dermatomal pattern, which is just a fancy term for meaning like,
how does the nerve actually distribute?
So where do you feel it? So for instance, you could have a nerve issue
in your back and not have any back pain, but you could have, a numb
foot. And a lot of times this type of pain responds pretty well to like
locally targeted treatments like nerve blocks and such like that.
Nosoplastic pain arises from altered nociception, but without clear
evidence of actual or threatened tissue damage. So like more
ambiguous. One presenter called it a volume control problem or
amplification issue. And it's usually a global problem, which means that
it's like widespread. And one presenters noted it's not just affecting pain,
but also sensitivity to light to hearing.
Right. I'm sure a lot of us have the, have that as well. So examples of
this are migraine headaches, fibromyalgia, pain reported by patients with
rheumatic disease is also in combination, often in combination. So not
just one type of pain, right? So we get multiple and they're combined and
they evolve over time.
And there was a new study, which was just published earlier this year,
which was so really interesting. That looked at patients with RA who had low inflammation. It looked like their disease status was pretty stable,
like well controlled. And, and they said, let's look at their, like their joint
fluid, right?
Let's pull out fluid from their joint and just look at it. So they actually
found a certain gene module, which had, I'm sorry, 800 different
combinations. And they said that was pretty consistent in all the
subjects, and they took these cells and put them in culture in a lab, and
the cells actually grew new nerve endings.
So this was so interesting, and again, that's really all the information I, I
have on it cause that's all really the presenter noted. But something I
want to mention, cause I think we'll be hearing about that in the future.
So at different conferences. This same presenter also noted that studies
show JAK inhibitors tend to improve pain better than some of the other
biologics like TNFs.
And she said again that traditional lab tests or even assessment tools
like looking at swollen joints tend may not be reflective of the amount of
pain a person is experiencing. A term, co culminant fibromyalgia, was
mentioned, and this basically means that there's a significant amount of
fibromyalgia that occurs in RMD patients, particularly inflammatory,
inflammatory rheumatic diseases.
And studies show that this happens about 20% of the time, and really,
like the general public, about 2% of the time. So something to really
think about. One presenter talked about primary versus secondary
fibromyalgia. And this basically has to do with which nerve pathways are
affected. And she didn't say the symptoms are different in any one or
worse than any one type.
She did say that if the product provider can figure out which pathway is a
culprit, there are different medications which could be effective, more
effective for one than the other, so that was pretty cool. There is a high
rate of being diagnosed with fibromyalgia in the first 12 months of being
diagnosed with a newly discovered inflammatory disease, and that also
traditional inflammatory markers like CRPs that didn't predict the
development of fibromyalgia.
Going back to pain and fatigue, it looks like the research suggests if you
live in a wealthy country, you're more likely to experience pain and
fatigue than those living in a lower income country. And of course, this could be due to societal pressures on the individuals in that patients in
wealthier nations tend to really have higher health expectations.
So that was pretty interesting. There are steep consequences for the
medical under appreciation of fatigue and pain, including the delay of
diagnoses, impacts on quality of life, negative mental effects, anxiety,
depression, isolation, reduced work productivity, burden on the health
care system, society
really, awareness needs to be raised among patients and health care
providers, and multiple presenters said this. We have to educate both
communities on this prevalence and the significance of fatigue and pain,
and there needs to be an open communication between providers and
patients. And really that providers should not just be focusing on your
swollen joint or a traditional lab test, but really to incorporate
comprehensive tool assessments in clinical practice regarding fatigue
and pain, that these are really vital components of your overall health
and need to be considered.
So in medicine, we call these PROMs or patient reported outcome
measurements. So hopefully your providers are doing this with you.
These factors should really lead to a tailored treatment plan, which will
be different for everybody. And that plan should be made along with the
patient. And some of the treatments might be medicines, but others like
physiotherapy or cognitive therapies or other interventions should also
be considered.
So there's a lot and that's what I wanted to share with you today. Yes, I
will have another video on the remainder of that presentation, which was
just so fascinating. Again, I'm so excited to share this with you and thank
you for watching and I will see you soon.
[00:33:59] Tiffany: All right. And last, but certainly not least, we have
Leila Valente, who is our health education manager at AiArthritis.
And she is a person living with lupus nephritis, and Sjogren's disease,
and she is going to do an overview of brain fog. Woo! Yeah, that's a big
one, right? And it's exciting to know that there is research about these
symptoms, because this is a really, really big one that many of us
struggle with, regardless of our diagnosis.
We're going to turn it over to Leila.
[00:34:33] Leila: Hello, everybody. This is Leila, Health Education
Manager here at AiArthritis, and I am back again with my fourth debrief
and super excited to let you know about what I learned today. So I am
excited to talk to you about cognitive dysfunction because it is something
that so many people in our community experience and they also don't
know why it happens or what to do sometimes or how even to approach
it and it can be a very frustrating, thing to go through.
I personally have dealt with Cognitive dysfunction issues and so I will
talk a little bit about that throughout my debrief and the patient who
spoke she everything that she said resonated with me so much that I
made my husband watch part of the session because my cognitive
dysfunction has been very active the past few months and it's been a big
topic in my household.
So I am excited to basically talk to you about what has been said in this
session. So let's dive in. I thought it would be very helpful to share the
slides for this part of the debrief. So I'm going to go ahead and do that.
So she talks about how her level of cognitive functioning was before she
got diagnosed with her disease.
She was dealing with serious and time sensitive issues, working with
basically with CPS, like child protective services and responsibility for
vulnerable children and families, need to multitask, work under pressure,
ability to plan and organize, flexibility, focus, concentration, listening and
observing skills, and being attentive for and adapt to threatening or
escalating situations.
And after she talks about how her symptoms were all over the place. So
she did a little bit of like a visual exercise of showing how all over the
place our symptoms for cognitive dysfunction can be. I copied and
pasted a whole blurb of what she was saying, and I just wanted to
highlight a few things.
This is the part that really resonated with me. And when working on my
laptop, I'm very easily distracted. I'm pretty sure many people recognize
that. When I was still working as a counselor, I worked on three or four
different files at a time, and now I have to just take one task. And it's
difficult. I end up after 30 minutes, I look at it at the bottom of my screen
and there's 12 screens open and I started reading emails, started
replying to some of them, but never finished up and etc.
And even administration, like reading, filling in forms or reading
instructions or following steps in a procedure, they can really stress me
out to, acutely to the extent that I end up in tears or with an elevated
heart rate. So she talks here a little bit about the consequences of the
brain fog and the things that happen and I think really for me the feelings
of shame and failure frustration and denial and feeling insecure or
overconfident it's been really big for me.
And I think whenever I, I, I get stressed out so easily, I get
overstimulated, I have a hard time initiating tasks and I have to really
hype myself up to go ahead and start a task and it's been really hard.
And I actually, I tried to get tested for ADHD because I thought that's
what it was. And as we were going through the tests, we came to the
conclusion that it's all through cognitive dysfunction that all of these
things are happening.
So this really hits home for me, I totally understand what she's saying.
And here is the biggest part. What can we do about it? What helps her?
What can we try to organize our brain and help us make sure that we
don't forget things? And so taking breaks is very important, doing
puzzles slash memory games, plan my day and stick to it, developing
routines, work in silence or put a special playlist together that helps you
focus instead of distracts you, being physically active helps her as well.
Doing a to do list and prioritizing, asking for help or taking a step back,
being outdoors, shutting out sensory stimuli when tired, humor, and
putting things into perspective.
And it feels like she was talking to me during this session. So this has
been, this was a really good session for me. And for the patient session,
this is the rest of her, her take home points. So cognitive dysfunction can
show in many shapes and forms. The patient may not realize the extent
or may be overcompensating or masking symptoms.
It is up to the healthcare professionals to address the topic. Try not to
ask, but also look for the signs. A small problem may have huge impact.
Psychoeducation, informing and educating patients. Transcripts can help
empower them and dealing with cognitive dysfunction is hard work,
especially when already dealing with an RMD or an AiArthritis disease.
And so that was the patient's segment of the session. And I am going to
move on to the next part of the session. And this was a very interesting
diagram that the speaker showed. It's basically showing the correlations between all of these different symptoms and cognitive dysfunction and
how it can affect.
There's other factors like vitamin deficiencies, other diseases, but
everything that's on here can contribute to cognitive dysfunction. And
just trying to address all of those different things that can affect it. And so
this speaker tried to accumulate all of the different studies that had to do
with cognitive dysfunction in order to do a overview of recommendations
and explanation and management of cognitive dysfunction.
There are other things that you can check out just to double check if
there's something else wrong. If the signs of cognitive dysfunction are
happening, some things to look at, it could be any structural brain
alterations, cardiovascular, vitamin D deficiency, hypothyroidism, vitamin
V12 or folate deficiency, and the different drugs that can be causing this
such as antipsychotics or anything having codeine, benzodiazepines,
things like that.
The speaker also says that there aren't many studies just fully done on
cognitive dysfunction. Usually they're focusing on something else and
then they have cognitive dysfunction as part of their research. So there
aren't many cognitive dysfunction dedicated research studies. The
biggest thing that you can do to help manage cognitive dysfunction
though, is treating the underlying disease.
I tend to see that whenever my infusion is due, within like maybe three
or four days, is when my brain fog is at its peak. Either that or when I'm
extremely stressed out and I know that I can probably be flaring. So
either in a flare or right before I need my infusion is when I am usually
experiencing more intense cognitive dysfunction.
So making sure that you treat the underlying disease is the main thing
that you can do. They also do talk about recommending to see an
occupational therapy, seeing if your insurance would pay for an
occupational therapy to help you with trying to cope with all of these
different symptoms and how it affects your daily life and coming up with
those routines with you and coming up with mechanisms in order to
remember things.
That's what occupational therapists do. They help us to live our everyday
life with whatever ailment we may have at that time. And the conclusion
from this segment was results tentatively indicate that levels and change of cognitive dysfunction correlate with fatigue, pain, physical inactivity,
psychological distress, and sleep problems and treating those
associated factors according to existing recommendations are points to
consider.
So if you're not sleeping well, if you have anxiety and depression, those
can definitely exacerbate your cognitive dysfunction as well as fatigue
and pain and any inactivity with exercising and things like that. The last
segment talks about very specific screening tools. So they bring up three
different screening tools, which is one, the Mini Mental State
Examination, two, the Adenbrooks Cognitive Examination, Number three
and the Montreal Cognitive Assessment test or the MOCA test. And with
the Mini mental state examination, I am familiar with that because it used
to work in senior care. So that is used a lot for seniors and for dementia
testing. And so another self report tool is mostly our questionnaires. And
this one is called MASQ, M A S Q. And it's the multiple abilities self
report questionnaire. It's a 38 item measure of self perception of
cognitive difficulties, and it focuses on language, visio perception, verbal
memory, visual memory, and attention and concentration.
And so that can still be a hard task for some people to take because it is
extensive. It's 38 items. And so they also did mention another one that's
called the Multidimensional Inventory of Subjective Cognitive Impairment
or MISCI, M I S C I. There's 10 items on there, and you basically rate
them. And it has to do with, clearly thinking without extra effort, mind
being sharp, remembering things, concentrating, shifting back and forth
between activities. That's a really big one for me. It says I have had
trouble shifting back and forth between different activities that require
thinking. I call it a buffer time, but usually my buffer time between
switching tasks is anywhere between 10 to 20 minutes and it can be
very frustrating to have to re center myself again.
Having trouble planning out the steps of a task, that is always very hard
for me as well. And trouble finding the right words or trouble expressing
myself clearly. So those are like the indicators of this test on whether or
not someone is experiencing mild, moderate, or not. extreme or severe
cognitive dysfunction.
Focus on the impact of the cognitive dysfunction and the management of
the other variables and not so much the actual symptoms but helping to
manage what the symptoms cause because unfortunately there is not
much that we can do or that we have found that we can do to help treat cognitive dysfunction besides treating underlying conditions and learning
how to cope with it. And so that was my debrief for today. I hope that you
enjoyed it and that you learned something or at least felt heard. If
cognitive dysfunction is something that you might be experiencing, I
know it could be very lonely and isolating, but it's good to know that they
are starting to do some research in this sector and hopefully in the next
few years we might even have a medication or something else that
explains or helps with cognitive dysfunction.
Thank you again for joining us this time around for our Go With Us
Program to Eular 2024. Thank you so much again, and I will see you
later. Bye.
[00:46:23] Tiffany: Okay, well, that was a sample, just a sample, of what
you can learn when you go with us to conferences, going with AiArthritis,
your peers, patients, to these conferences.
And we have another one coming up, we, every year, ACR November,
EULAR June, so make sure you go to AiArthritis.org/conferences there
you'll be able to get a link to all of our debriefs, not just from EULAR
2024, but all of the times we've gone in the past. So there's literally,
literally hundreds of resources that you can pull from these videos from
these debriefs. Also, if you go with us to conferences, there are two
ways that you can get involved. You can sign up for the daily debrief. So
you would get links to the videos and the recordings that you had just
heard or seen, depending on how you're participating today.
But also you have an elevated experience. Everything we do at
AiArthritis has the option of an elevated experience, which means you
can get more involved in activities to improve your health care journey.
In this case, you can sign up to be zapped into a slack channel. And
from there, you will be able to actually talk to myself and the other
people who go in person and ask questions.
We do behind the scenes videos, talk to researchers, talk to other
nonprofits, other advocates that might be there. It's a really unique
experience and it's free. So we definitely encourage you to sign up for
that. And also, while you're on the site, please consider a donation to the
organization.
We work hard each and every day to make sure that we're bringing the
best resources, the best patient developed resources and patient opportunities, patient led opportunities to use to improve your life and
the lives of the millions of people around the world living with our
diseases. And there you go.
That is a wrap. Signing off from Aiarthritis Voices 360. Have a fabulous
rest of your day.
Aiarthritis Voices 360 is produced by the International Heart Association.
Foundation for autoimmune and autoinflammatory arthritis. Find us on
the web at www.AiArthritis.org. Also, be sure to subscribe to this podcast
and stay up to date on all the latest AiArthritis news and events.
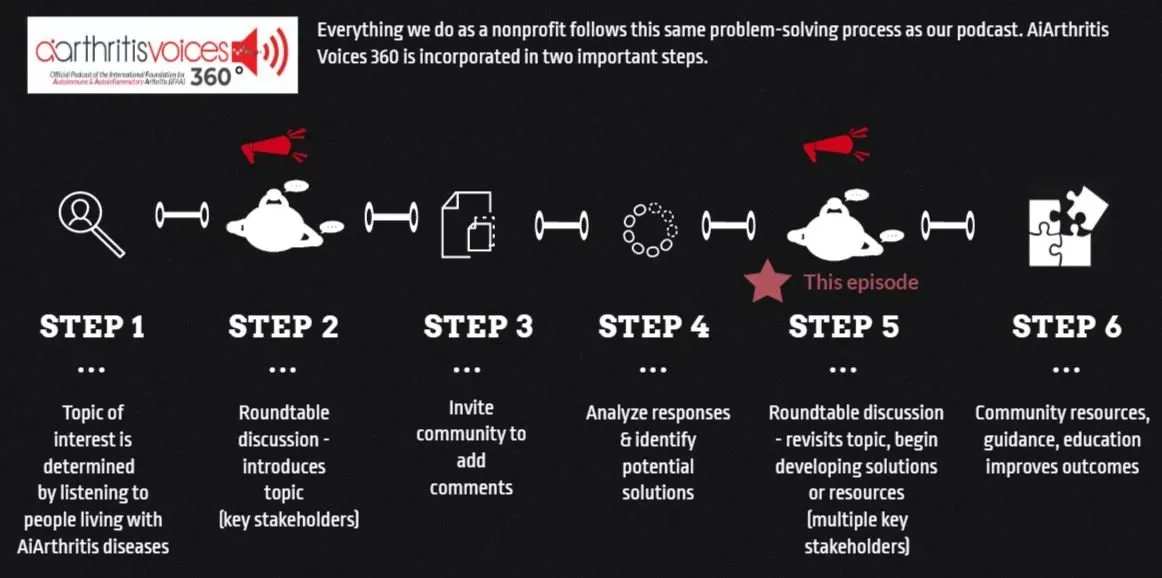
All our main 1st Sunday of the month episodes are either an initial "put the topic on the table" episode (Step 2 in our organization's 6-step problem solving process) or a "revisit to the table" episode (Step 6 in our organization's 6-step process), where we build on a past show because we have moved forward in developing help, tools, or projects around the issue (Step 5 in our organization's 6-step process).
After each show airs we spin off the conversation into many discussions over various formats, which we now call #360its (new in 2022)!
-
Additional Resources & Information
- Volunteer with AiArthritis : https://bit.ly/AiArthritisVolunteerApp
- Donate to Support the Show: https://www.aiarthritis.org/donate
- Follow AiArthritis on all social media platforms @IFAiArthritis
- Sign up for our Monthly AiArthritis Voices 360 Talk Show newsletter! HERE
New Title
Leila P.L. Valete
Leila is the Health Education Manager at the International Foundation for AiArthritis. She is a person living with Lupus Nephritis and Sjögren’s Syndrome. She is passionate about inclusion and diversity in health education and meeting individuals where they are at in order to learn in a way that resonates with them. Leila is on social media as @LupusLifestyle.Lei sharing bits and pieces about her life with lupus and connecting with others. Connect with her on Instagram or TikTok.
Connect with Leila:
- Instagram: @lupus.lifestyle.lei
- TikTok:
@lupus.lifestyle.lei
Tiffany Westrich-Robertson
Tiffany is the CEO at AiArthritis (International Foundation for Autoimmune & Autoinflammatory Arthritis) and uses her professional expertise in mind-mapping and problem solving to help others, like her, who live with AiArthritis diseases work in unison to identify and solve unresolved community issues.
Connect with Tiffany:
- Facebook: @tiffanyAiArthritis
- Twitter: @TiffWRobertson
- LinkedIn: @TiffanyWestrichRobertson
Deb Constien
Deb is a medically retired Registered Dietitian and a Representative for the AiArthritis with Rheumatoid Arthritis. Deb is also on the Advisory Council for WREN- Wisconsin Research Education Network and a Patient Family Advisor- PFA on an International PCORI research study for ACP- Advanced Care Planning.
Connect with Deb:
- Facebook: @deb.majcherconstien
- Twitter: @debconstien
- Instagram: @debconstien
Pull up your seat at the table
Now it's YOUR TURN to join the conversation!
What do you think about this episode?
We want to know what you think! By continuing the conversation with your opinions and perspectives - we all get a better understanding of the problems facing our community. Better yet, through these conversations we can start working and developing solutions.
We mean it when say 360. Not only do we want your input anytime and anywhere, but we also are eager to see where the conversation will take us. So please, "pull up a seat at the table" and let's start talking!
Email us at podcast@aiarthritis.org, message us on social media (find us by searching for @IFAiArthritis)
Relevant Episodes & Projects
Episode 62: Patient-Reported EULAR2021 Debriefs ... and We're Off!
This week join your patient co-hosts Tiffany Westrich-Robertson, Deb Constien, Katie Simons and Patrice Johnson as they brief our AiArthritis patient community on the first day of EULAR 2021 with patient guest Leslie Rott Welsbacher.
Episode 58: Diet, Research, & AiArthritis - an ACR Special Presentation
Join your patient co-hosts Deb Constien, Tiffany Westrich-Robertson, and Patrice Johnson as they take us backstage at the American College of Rheumatology (ACR) Annual Conference as Deb introduces a research review from the ACR about diet.
Episode 40: Research at a Glance - Posters & Abstracts: Patient reviewers, here we come!
Join TIffany as she talks about the importance for both patients and organizations to review Posters/Abstracts and invites all patients to join her to continue the reviews as part of our "Go with Us" to EULAR 2020 initiative.
Love the show? Help us make sure we stay on the air by making a donation.
Your contribution helps us continue the work we do every day to improve the lives of millions worldwide.