Relapsing Polychondritis (RP)
How to pronounce it:
Relapsing -
ree-lap-sing, Polychondritis -
pah-lee-cawn-drEYE-tis
AiArthritis defines Relapsing Polychondritis as:
Relapsing Polychondritis (RP) is a rare autoimmune disease that causes inflammation of cartilage in the body. It most commonly affects the ears, nose, airways, and joints but can also involve the eyes, heart, and brain.
Symptoms & Characteristics
Common in All AiArthritis Diseases
Flares: Periods of worsening symptoms are called flares. A flare can last for hours, days, weeks, or months.
Physical Activity: Condition improves with activity and exercise and worsens with rest.
Comorbidities: When inflammation is left uncontrolled due to lack of proper treatment, comorbidities can develop. 70% of patients with chronic, lifelong disease will develop comorbidities, including dual or triple diagnoses.
Family History:
Autoimmune diseases often run in families, indicating a potential genetic predisposition where that gene can cause disease. Autoinflammatory diseases can occur multiple times in a family, but is based off of genetic mutation. It is not a gene that causes the disease— but a mutation on the gene that can cause the disease which can then be passed on to the next generation.
"Auto" Symptoms
Fatigue: Severe fatigue or exhaustion that may not be helped by caffeine/stimulants and can happen even after a long period of rest.
Cognitive Dysfunction: Brain fog or periods of time where thinking gets clouded and it becomes difficult to concentrate.
Flu-like symptoms: Without having the flu- nausea, muscle weakness, and general malaise.
Fever: Typically low grade in autoimmune (with exception of juvenile idiopathic arthritis) and higher grade in autoinflammatory (% strongly varies per disease).
Reference: Early Symptoms of AiArthritis Study, AiArthritis, 2019.
Inflammatory Arthritis Symptoms
Stiffness: Severe stiffness in one or more joints, especially in the morning or after sitting for long periods of time.
Joint Pain: Episodes of joint pain that may last for hours, days, or even weeks, that can appear and disappear suddenly. Often described as “jumping pain” into different locations.
Typically the joint pain will coincide with one or more “Auto” symptoms and start and stop suddenly - for no apparent reason (which is called a "flare"). Some people will experience all of the above symptoms, others only a few.
If you have any of the arthritis features, and at least one of the “Auto” features, please consult your physician about a referral to a specialist.
Symptoms Often Associated with Relapsing Polychondritis
- Inflammation, redness, swelling, or pain of the outer ear
- Hearing loss, tinnitus, or ringing in the ears
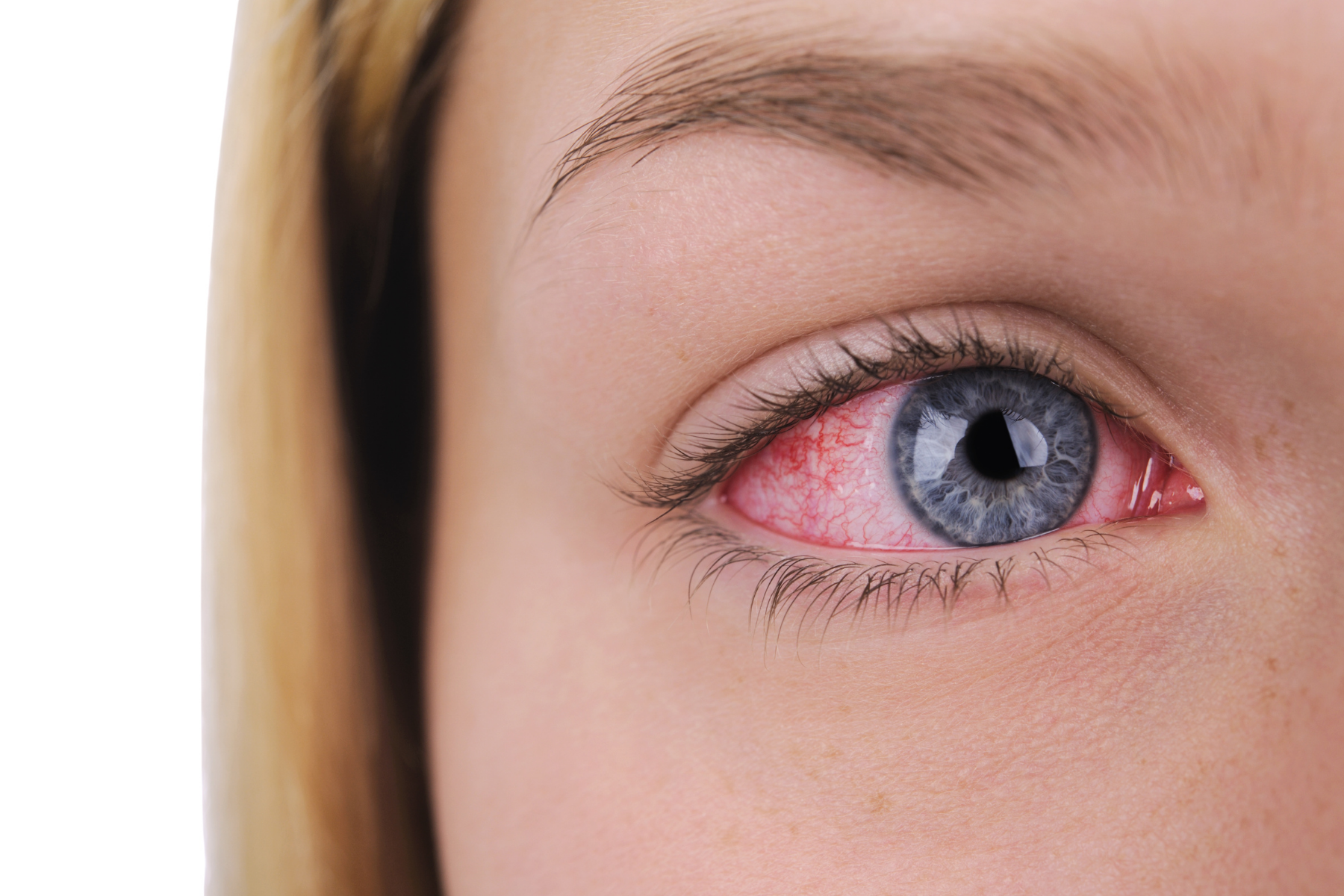
- Redness and pain in the eyes
- Sore throat, neck pain, or a hoarse voice
- Shortness of breath, wheezing, or a dry cough
- Pain and redness of the nose
- Skin lesions
- Rib or sternum pain
- Stridor (high-pitched sound during breathing)
- Leaky heart valves
- Kidney disease
- Nerve problems
- Tissue damage causing deformity and poor functioning
Diagnosing Relapsing Polychondritis
There’s no single definitive test that can confirm a relapsing polychondritis diagnosis, so rheumatologists look at a combination of physical exam, blood tests (ESR, WBC, RBC), and imaging, along with a family history of autoimmune or autoinflammatory disease.
Relapsing polychondritis is diagnosed when a doctor observes at least three of the following symptoms developing over time:
- Inflammation of both outer ears
- Painful swelling in several joints
- Inflammation of the cartilage in the nose
- Inflammation of the eye
- Cartilage damage in the respiratory tract
- Hearing or balance problems
Relapsing Polychondritis Treatment Options
Treatment OptionsTreatments are tailored to each individual's disease, but visit our Treatment Options page to learn more about the different types of treatments that are used for Relapsing Polychondritis.
What Fellow Relapsing Polychondritis Patients Want You to Know
Submit YOUR AdviceWe need YOUR advice! Fill out this form to give peer advice to those with your disease.
Interesting Facts about Relapsing Polychondritis
- Relapsing polychondritis was first described in 1923 by Dr. Jaksch-Wartenhorst, who identified recurrent inflammation of cartilage in various parts of the body, including the ears and nose. The name “relapsing” reflects the episodic nature of the disease, while “polychondritis” refers to inflammation of multiple areas of cartilage. Its cause remained unclear for many years, but it is now known to be an autoimmune condition.
- Relapsing Polychondritis can often be mistaken for an insect bite or an infection, leading to an incorrect diagnosis and a prescription for antibiotics.
- Relapsing Polychondritis does not appear to run in families, although some people may have genes that increase their risk of developing the disease.
Relapsing Polychondritis Awareness Days/Months
- World Autoimmune and Autoinflammatory Arthritis Day - May 20th
- Rare Disease Day - February 29th (28th)
- Autoimmune Awareness Month - March
- Rheumatic Disease Awareness Month - September
- Pain Awareness Month - September
- Chronic Disease Awareness Day - July 10th
- Invisible Disabilities Week - 3rd full week of October
Other Relapsing Polychondritis Resources
In an effort to ensure this page has the most accurate and up-to-date information, this page is currently awaiting medical review. Some information is subject to change.
Page Last Updated: 10/24/2024