It's More Than in Your Head-- Neurological Manifestations of Sjögren's and Lupus with Dr. Julius Birnbaum
AiArthritis Voices 360 Main, Full Episode 108
Air Date: April 6, 2025
This episode is a Step 2, as outlined in our 6 Step Patient-Led Problem Solving Process.
Autoimmune diseases like lupus and Sjogren’s disease are often associated with joint pain, fatigue, and organ involvement, but their impact on the nervous system is less commonly discussed. In this episode, Dr. Julius Birnbaum, a leading expert in neuro-rheumatology, joins us to explore the neurological manifestations of these conditions and what patients need to know.
From brain fog and memory issues to more severe complications like neuropathy, Dr. Birnbaum explains how these diseases affect the brain and nerves, why symptoms can be challenging to diagnose, and the latest advancements in treatment.
If you or a loved one live with lupus or Sjogren’s and have experienced unexplained neurological symptoms, this episode provides clarity, validation, and expert insights on what to look for and how to advocate for proper care.
Discover Dr. Julius Birnbaum's newly released book, Living Well With Autoimmune Diseases: A Rheumatologist’s Guide to Taking Charge of Your Health
- Help us DRIVE AWARENESS for World AiArthritis Day 2025 (May 20th)
- Donate for World AiArthritis Day or start YOUR OWN race team
Episode Highlights:
- Understanding the link between AiArthritis diseases and the nervous system.
- Common neurological symptoms in lupus and Sjogren’s
- Why neurological symptoms are often overlooked or misdiagnosed.
- The latest research and treatment approaches for managing neurological complications.
- How to advocate for proper testing and care if you suspect neurological involvement.
AiArthritis Voices 360 is produced by the International Foundation for Autoimmune and Autoinflammatory Arthritis. Visit us on the web at
www.aiarthritis.org/talkshow. Find us on Twitter, Instagram, TikTok, or Facebook (@IFAiArthritis) or email us (podcast@aiarthritis.org). Be sure to check out our top-rated show on
Feedspot!
Follow
AiArthritis on all social media platforms
-
Expand to View the Podcast Transcript
Episode 108
Leila: [00:00:00] Hello everyone and welcome to AiArthritis Voices 360. This is the official talk show for the International Foundation for Autoimmune and Autoinflammatory Arthritis or AiArthritis for short. My name is Leila P.L. Valete, and I'm a person living with Lupus and Sjogren's Disease, and I am the health education manager here at AiArthritis.
Today I have a special guest joining me, Dr. Julius Birnbaum. I'm met Julius this past ACR as he was going around to the different booths. And he let me know that he was publishing a book for patients, and I knew I wanted to get him on the talk show to talk more about it. Here at AiArthritis Voices 360 Talk show, we have an equal seat at the table as experts in our disease as patients.
So we are a little bit more informal and we like to go on a first name basis with our guests and
[00:01:00] co-hosts who are also doctors. So, Julius, please let us know a little bit more about you
Dr. Julius: for sure. So I, happy to be her on the show. I start with, I have a lovely wife and three children. Jeremy, Aaron, Samantha, and I will say as a result of this book, they now think that I know a fraction of what I'm talking about.
So that's been one of the gratifying benefits of the book. Originally I grew up in New York City. I've lived there for 30. I moved on to Johns Hopkins in Baltimore where I did my fellowship, and right now I'm at the University of Pittsburgh Medical Center in Pittsburgh, and I've been here for four years.
Love it a lot.
Leila: Awesome. And I know that we're gonna be talking a little bit about the neurological manifestations of Lupus and Sjogren's. So, why don't you tell the audience a little bit about how you have such a big emphasis in
[00:02:00] neurology?
Dr. Julius: Sure. So I, I, I initially did my residency in neurology.
And at the end of my neurology residency the last year, I started taking care of patients with a lot of fascinating complications, rheumatic diseases. So this included lupus patients with a lot of brain lesions and included Sjogren's, patient with painful disorders, rheumatoid arthritis, patients with spinal cord injury.
I realized if I wanted to take care of these patients, I needed to have a broader understanding of how these diseases not just affected the brain, but the heart, the lung and kidney as well. So I returned and I did an internal medicine residency, and subsequent to that I completed a rheumatology fellowship at Johns Hopkins Hospital.
So I told this was more than nine years of training after medical school, but I thought it was well worth it. And when I [00:03:00] was at Hopkins, I managed to combine my training in a synergistic way. So I was able to open up what I termed the neuro rheumatology clinic, and that's when I had a unique opportunity to care for patients with diseases at the interface between neurology, rheumatology.
Leila: That's awesome. I think one of the biggest things that air arthritis that we always try to emphasize is that arthritis, the arthritis that we're talking about is a, is a systemic disease. So knowing that, like you said, every different organ, including the brain and all of the different parts of the body can be affected.
So, it's really cool to see how you got your path to having the intersection of rheumatology and neurology. And I think specifically right now, a lot of the hot topics that patients are talking about have to do with brain fog, fatigue, pain and all of these have to do with neurology as well. So it's gonna be so interesting to hear a little bit more about what you have to [00:04:00] say.
And so during our first meeting, you told me that you wanted to discuss the intersection of rheumatology and neurology, specifically in lupus and as in Lupus and Sjogren's, and as a lupus and Sjogren's patient myself, of course, I was definitely interested in hearing more specifically, like I said, yeah, a lot of people in our community are dealing with brain fog, fatigue, mental health issues, and those are like the really heavy topics day to day because it affects your day-to-day life so much. And sometimes we don't get a lot of advice on, on how to deal with those specific symptoms. So, I'm sure that, you know, getting some background on them and maybe a little bit of advice from you will be super important. And I think what's really cool about this as well is that for the past year we've been creating these different resources on the different.
Stops of the patient journey and this this information will definitely be able to fit into either the coexisting conditions [00:05:00] section or even just, you know, living with the disease, which has to do also with progression of the disease and different side effects that come with that. So, that'll be amazing.
And so, maybe you can start with telling us a little bit about the neurological side effects of Sjogren's specifically, and I know that in the Sjogren's section of your book you talk a lot about neuropathies. Can you tell me a little bit about what that means?
Dr. Julius: So, sure. So when neurologists use the term peripheral neuropathies.
What's imply is a certain anatomy. So the peripheral nerves, for example, connect the spinal cord to the skin to muscles. And when the peripheral nerves can become injured, it could cause weakness, but also a lot of what we call sensory symptoms, such as numbness and tingling. And there are also particular neuropathies, which are called small fiber neuropathies, which particularly cause a lot of neuropathic [00:06:00] pain.
So when I say neuropathic pain, patients might experience burning pain. Patients might experience shot like sensation and patients might also experience extreme exquisite to touch. So for example, bedsheets at night where you can get their feet can cause intolerable pain. So these are the type of pain that could occur in neuropathies and refer to them as painful neuropathies.
Leila: That's really interesting because I actually, I went to a talk at this past ACR as well, that was about pain and talking about the different types of pain. You know, neuro neuropathies being a type of them basically saying like some of the pain that AiArthritis patients or patients with these rheumatic diseases may have, may also be very similar to the type that f fibromyalgia patients have, which kind of seems like it's tying in similarly to what you're talking about with the peripheral neuropathy.
I never really knew that peripheral [00:07:00] neuropathy was, was an exact symptom or could happen from lupus. But the first time that I had a really big flare, they put me on gabapentin because I was having pins and needles. I was having all of this go on with my nervous system that I didn't really understand what was happening.
But now that I put the two things together, I think that's what was happening, is that, that there was some neuropathy, pain going on at that point when I was having that first big flare with lupus.
Dr. Julius: Yeah. And the neuro just saying the neuropathy pain can be somewhat amorphous and, and, and difficult to understand because it's assault and so many different sensory symptoms.
And the sensory symptoms can present with such an incredible heterogeneity of symptoms to, like you're describing with yourself, like the tingling, the numbness, you know, that can happen. I think what happens also is that patients resort to language, language could actually be, you know, exquisitely lyrical.
So [00:08:00] I've had patients tell me that, you know, someone's taking a blowtorch to, to my feet or you know, their feet are open when they're going in a body of ocean. And I think that when you use this intense language, what you're trying to do is convey to your physicians how much they're suffering. And physicians by their training are used to telltale terms like tingling, numbness, so sometimes going off script and becoming more adept and understanding how these are personalized to you, that could actually lead to some symptoms becoming marginalized and even undiagnosed in certain ways.
Leila: Definitely, I, I just had a discussion with some of our volunteers about this exact thing, about one of the resources we should come up with is the different de descrip description words on how to describe your pain so that you can be a little bit more detailed when talking to your physicians, because that may be part of the problem is just the [00:09:00] breakdown in communication of what you were talking about. And basically like to kind of go into it a little bit more of a breakdown. There's a difference in the pain that we're talking about of like the numbness, tingling, burning versus a mechanical pain that may happen say if you sprain your ankle or if you have some other acute injury, the, the, the descriptor the description words would be completely different. You'd be, it'd be a sharp, tight pain. Exactly. You know, exactly. When it comes to the, you know, spraining your ankle or breaking your arm and those, that's really important for patients to have the, that language that you're talking about, to be able to communicate what they're trying to say to the pa, to the doctors.
Dr. Julius: Yeah. I think you're right. You know, we use the term inflammatory pain. So like when you're seeing your ankle, and it might be a sprain like you're talking about, you'll see redness, you'll see warmth, you might see a bruise, so you could see the actual injury itself. When you have neuropathic pain, [00:10:00] there's nothing that visibly you can see.
You see your skin. And patients a lot of times understand and they don't understand why it's so enigmatic, like where is it coming from? Where is the pain generator? So it's important to understand that in neuropathy, it's the nerves inside that connect muscles to spinal cord, spinal cord to skin. So you're right, there's a big, big difference between what you can see in inflammatory pain, like when you spread in your ankle versus a neuropathic pain, which is actually invisible to the eye.
Leila: Yes, and we talk, you know, a, a lot of these different diseases are invisible, like what you said. And so it can be really tough even for patients themselves. You're like, am I really experiencing this pain? What is happening? 'cause we can't see it. So I think that can be really tough for some patients to deal with.
And I think, like you were saying kind of go. Explaining the difference between the central and the peripheral [00:11:00] nervous system with the central being the brain and the spinal cord, and the peripheral nerves being everything else that is going to be connecting your body parts to the central nervous system.
And I think we talked a, we talked a little bit about the neuropathies in Sjogren's. How does that differ with Pat, with Sjogren's versus lupus? And I, I see that we may talk a lot about injury with spinal cords, with lupus as well like, is what, what's the, like, the breakdown of that?
Dr. Julius: Yeah, so I think that a lot of the neuropathies that are highlighted and more better about diagnosed in Sjogren's syndrome or Sjogren's disease, I should say, because Sjogren's has now appropriately changed its designation from a syndrome to a disease. I think that this reinforces to rheumatology wider community, that it actually is something deservedly be called the disease.
So let me emphasize that myself. [00:12:00] Absolutely. So Sjogren's disease, it could cause a lot of different types of neuropathy. So the nerves themselves can be injured in different ways. So for example, we have tiny sized nerves that can be injured and when these tiny sized nerves are injured, this is what we call a small fiber neuropathy.
So again, the small fiber neuropathy gives ride to descriptors like we just talked about, burning pain shock-like sensation sensitivity to touch, and what happens and why small fibers neuropathies are undiagnosed, is that they require special diagnostic testing. So the diagnostic test of choice in a small fiber neuropathy is to take a, what we call a punch biopsy, which is a punch biopsy of the skin.
And then pathologists look at this biopsy under a microscope. And what they try to understand is if small fiber nerves are making it to the top layer of the schists, which is called the [00:13:00] epidermis. So what pathologists can see in a small fiber neuropathy is that these tiny nerves, they wiggle in the skin layer, but they never try to get to the epidermal layer.
So the epidermal layer is devoid of small fiber nerves, and this is what it's called, a decreased nerve fiber density in the epidermis. And that's kind of the buzzword that we use to describe small fiber neuropathies. It requires special tests, and until recently, it was not recognized that these special tests needed to be done for small fiber neuropathies.
Leila: Wow, that's amazing to hear about. I think that that's, we never hear about the, like the layers of what you're talking about when we think about our pain. And so I think just even understanding that information can help patients feel more empowered to talk about their symptoms and and feel like it's a real thing as well.
Dr. Julius: Yeah, and what we do in our manuscripts, our research studies [00:14:00] is we actually try to get the biopsy slides and put into pictures what pathologists are seeing because you're right, I think it's very, very powerful to patients that they could have a certain anatomical locus and they could say, ah, here's where my nerves are not working as where they should.
So once you have a visible portrait of how you small fiber neuropathies are being diagnosed, it helps reaffirm to you that, Hey, what I'm experiencing is real and organic, and it's not just in my head.
Leila: Like with lupus nephritis, you could get the biopsy of the kidney and you know exactly what class it's gonna be.
So it's like very similar. It's taking it as, you know, the same way like pain is being caused by these injuries and that's what's causing it. So I think that that, like you said, like we both said, it's very empowering. So we, yes, there. Is there any information that you have about lupus patients getting the injury to spinal cord?
Is there, is that a common thing [00:15:00] that happens?
Dr. Julius: So it's uncommon. And now it might only affect 1% to 2% of lupus patients. But here, why? It's really important because if you're a lupus spinal cord patient and it's not treated appropriately, unfortunately, you might spend a lifetime of irreversible paralysis and be relegated to a wheelchair.
So what I kind of discovered when I was at Hopkins, one of my initial research studies is that spinal cord injury in lupus is actually quite heterogeneous. So it's not just one type of spinal cord, a injury, it's actually two. So the first type of spinal cord injury that was undiagnosed and underrecognized is what we call the gray matter variant of lupus myelitis. So we say gray matter because it affects the central part of the spinal cord where there's a lot of nerve bodies. And what we identified was that this gray matter myelitis was [00:16:00] actually not inflammation of the spinal cord, but it was actually a spinal cord stroke.
Oh, wow. So if you suffered, yep. If you suffered an I spinal cord stroke, that's why you're gonna be so decimated. We identified also that there's a crucial warning sign. So all of our patients with Brain Matter myelitis, they had this prodrome where they were unable to urinate for hours or even days beforehand, and often they were misdiagnosed as having a urinary tract infection.
And this is what we identify that if you had a lupus patient come in without another cause for being challenging to void, difficult to void, that this was your warning period. And if you intervene with high dose steroids at this time, you could prevent patients from suffering a lifetime of being unable to walk and being relegated to a wheelchair.
So as the gray Matter event Yeah. It, it's a, it's a stroke, but, but the good thing is that we recognize that it's, [00:17:00] there's warning signs and, and ways to intervene. So.
Leila: Exactly. Yeah. I mean, if it's, like you said, if it's, if you can take a high dose of steroids to totally, you know, avoid that for at least, or at least postpone it for the time and try and figure out what's going on.
That is so important for er doctors and primary care doctors to maybe know you know, if one, if they have a lupus patient just in case, even though it's only 1% or 2% that it may happen to.
Dr. Julius: No, exactly. And then we also identified that there's a different pattern of spinal cord disease, and we called it the white matter variety because it tends to affect the myelin coating that's on the outside of the spinal cord. But one myth that we were able to debunk is that for a long time, a lot of physicians thought that multiple sclerosis was a type of complication that can occur in lupus patients. And what we identified that multiple sclerosis was actually extraordinarily rare in [00:18:00] lupus patients with spinal cord disease.
Instead, they were affected by white matter and the initial attacks could be quite severe. It could still affect the nerves and muscles. Patients could still be relegated to wheelchairs, and this is after a few attacks. In multiple sclerosis, in contrast, you could develop similar weakness, but whereas the white matter variety in lupus can lead to spinal cord injury and maybe wheelchair dependence within five to 10 years.
Similarly. Multiple sclerosis patients can have slower evolution of weakness. So again, this was the second myth that we tried to debunk and that multiple sclerosis is actually very, very uncommon as a manifestation of lupus, especially the spinal cord injury. So these two different types of spinal cord injury each different in of themselves, but each of them much, much different than multiple sclerosis.
Leila: [00:19:00] Wow. Yeah, I mean, I can totally see how people might have, you know, confused the two for a little bit, but that totally makes sense that it's, you know, just, you know, the different inflammation on the different parts of the spinal cord. I, I have a question about like SLE, like systemic lupus like progressing into CNS lupus or, or, you know, lupus that affects the the, you know, like the neurological side. How often does that happen for someone who has SLE or like, if someone's, you know, control, you know, usually controlled, like for me, I'm on benlysta and hydroxychloroquine and that's kind of it and I've been stable for a few years. How common is it for there still to be, peripheral manifestations and then central manifestations of lupus to come if, if my inflammation is quote unquote controlled for the most part?
Dr. Julius: Yeah, I think that's a great question. I think for the most part, if your lupus complications are [00:20:00] controlled experience, you know, if you have initial lung or kidney joint or, or, or heart disease.
If you are able to tamp down the ferocity and the inflammation of these organs, the neurological complications actually due to lupus are less commonly to occur. Now, I wanna emphasize when I say neurological complications due to lupus, because also what we've identified is that neurological complications can occur in lupus, but actually the majority of lupus complications can stem from non lupus origin.
So, for example, you might have fatigue, and that could be associated with medications. It could be associated with disorders of, of glands, such as the thyroid glands. And, and these are not directly due to lupus. So when you have neurological complications that occur after, if your lupus had been [00:21:00] effectively treated, you could still develop neurological complications, but they might not directly stem from lupus.
Leila: And I think that that can also be something that happens, is that whenever you go to the doctor and they say, and you say like, I have this going on. I have that going on, it, I feel like sometimes there could be a blanket of, oh yeah, that's, that's a, that's a side effect of lupus. That's a side effect of your lupus.
I feel like I hear that a lot and I'm like, I just wanna bring it up because maybe it's not the lupus, maybe it's something else. And I feel like that need, like you said, it should be emphasized that rheumatologists and primary care doctors should know that and should be trained to look for the non lupus origins of some of these different symptoms that may be happening.
Dr. Julius: I think that's so true. And, and I think what happens without being pejorative is that a lot of physicians can be so overwhelmed by these neurological complications. So let's say for example, a lupus patient develops [00:22:00] seizures, and you know, the le the seizures can be due to an infection. The seizures can be due to kidney disease, which is not necessarily active at that point.
Seizures might stem from disorders that can increase or lower sodium, but they're scary to see. So when you have someone with seizures, you know there's seismic shaking of the arms and legs. So if you have a lupus patient with seizures, I would say, Hey, this is so overwhelming. Who wouldn't say that's not due to seizures?
And a lot of patients are apparently sometimes put on immunosuppressive medications for neurological disorders. Even though those neurological disorders are not due to lupus. So what happens in the case is that the immunosuppressive medications at best are not effective or at worse, making more crohn to infections.
Leila: Definitely. Yeah. That is so interesting to hear about. And I think that, just this information, being [00:23:00] able to get that information out there that you were saying about debunking whether MS is a, you know, an escalation of lupus symptoms and, and all of this is a really good place for patients to kind of start to understand the neurological side.
It's something that we are not often warned about, or told about on an every, you know, visit basis. It's not like, hey you know, make sure that you check out for these specific symptoms when you come back, and all of this kind of stuff. So it's I think that that's something that we can also maybe give some advice on is what symptoms may come up that patients can look out for where it is a, is a warning sign, like you said, with the, with you know, not urinating for a few days for for the spinal cord injury. Is there any other general symptoms that you can let patients know that might be a warning sign that there may be something going on on the neurological side for lupus or Sjogren's?
Dr. Julius: Well, I think one of [00:24:00] the things that's recognized is what are your symptoms, again, like we talked about of a neuropathy. So again, being very at tuned to your body and noting whether you're having any central or symptoms, pain symptoms, and trying to identify it at this earlier and more incipient phase because you're gonna know your body better than physicians.
So I think in a sense you wanna be cognizant of the fact that the neurological complications can occur in a wide variety of ways. Being sensitive to your body, knowing any perturbations or, or changes, I think that's the the biggest goal. And it's in turn like knowing your body, having the conviction that something is dissimilar to you, and then also having the conviction that, hey, this is something that I really think is important that I should report to my physicians.
Leila: Definitely, like you said with any shocking feeling or snapping [00:25:00] feeling, the warm, or sorry, not warmness. We were saying, oh yeah, like, like warmness as well like any type of if you look up the information for nerve pain right there can be some descriptive words that you can look up to see if that may be what you're feeling.
If it's not necessarily aching pain that you usually feel on an everyday basis with your lupus, that can kind of be a sign. Okay. Let's see. We did touch about this a little bit more, a little bit in the beginning. This brain fog symptom that, you know, everybody. Feels like they have at some point with lupus and Sjogren's.
There's a lot of talk about brain fog. The, you know, the scientific name that we use is cognitive dysfunction. What is the connection between brain fog and, and these diseases? And is there anything that you can recommend for brain fog?
Dr. Julius: Yeah, and I think when we use the term brain fog, you know, that's an incredibly descriptive symptom [00:26:00] that might explain some of the underlying mechanisms. So again, brain fog is a metaphor and right away you described something that's very incisive, and I think your physician will recognize this as a common symptom. So when we think about cognitive impairment, we try to think about whether the cognitive impairment is affecting certain anatomical loci at the top of the brain, which is called the cortex, or the under part of the brain, which is called the sub cortex.
So, for example, when we talk about Alzheimer's disease, this affects the cortex of the disease and it's certain deficits, which I call the a. So aphasia difficulty with speaking aleia, difficulty reading a calcula, difficulty calculating. So there's an a pattern of deficits that occur in what we call the cortical cognitive impairment, like Alzheimer's.
So what fortunately happens in lupus is this [00:27:00] is important to def emphasize, it's not a neurodegenerative disease. So you're not gonna progress towards all the horror images that you might know if you had a older loved one, a grandmother or grandfather with Alzheimer's disease. And I think that's one thing that can bring relief to my patients is I tell them, I'm not minimizing your cognitive impairment at all.
I wanna do is to tell you that cognitive impairment in lupus does not progress, and I, I have a colleague who had a research fund that was funded by the NIH and she wanted to use sophisticated imaging studies to see whether that a can predict certain types of cognitive impairment. The research study was really over in the first one or two years because here they had all these gorgeous tools to predict deterioration, but there was no deterioration.
And so that's become a little bit better known that [00:28:00] lupus cognitive impairment does not progress. Now, the other thing with the brain frog and similar, this is a theme that we've talked about is that in many lupus patients with brain fog, there's other underlying symptoms that are not strictly due to lupus.
So for example, fatigue is a debilitating cause of, of brain fog. And if you manage to try to elicit and treat some causes of the fatigue, the brain fog could get better. In addition to fatigue, pain can be an important correlate or, or associated with brain fog. So if you manage to treat the pain, the fatigue gets better.
Sleep disturbances can also be a cause of brain fog, and what I think is actually undiagnosed in lupus patients is sleep apnea. So sleep apnea can affect more obese patients, but not necessarily [00:29:00] it could affect patients who have normal weights. So you wanna have a partner who you could ask like, am I snoring a lot?
Do you hear me? Stop breathing at night? And that's regarded as sleep apnea. And I've seen a lot of patients with lupus cognitive impairment, who when identified as having some sleep disturbance and particularly sleep apnea, their cognitive impairment can get better quite quickly. And we talked about depression as another cause of brain fog.
So there's all these different contributors to brain fog in lupus patients. And again, I think that the central theme that we've been talking about is that all these symptoms that you can see in lupus, they might stem from non lupus causes.
Leila: Definitely, and I, I see that these three symptoms come sometimes bunched together when it comes to the ACR or EULAR with fatigue, pain and brain fog.
It seems like definitely what we're seeing is that there's a correlation between all [00:30:00] of them and kind of trying to isolate each individual symptom and trying to address that to see if it may help with the other symptoms seems like a really good way to address it with your healthcare providers and seeing how, like you said, if you can get better sleep, if that will help the fatigue and the brain fog. If you can you know figure out how much the pain how to, how to treat your pain. Then that may also help with the sleep and also help with the brain fog and fatigue. So there, it seems like, you know, everything with these diseases, everything's connected, it's all systemically connected. So just trying to to pinpoint what exactly may it may come from can be really difficult, but definitely worth the work to try to figure out in order to alleve those symptoms.
Dr. Julius: Absolutely, and I think what's interesting, we were talking about depression in, in lupus patients and the patients with rheumatic diseases. I, and I think it tends to be deprioritized for a variety [00:31:00] of reasons. You know, when you come to your physician's office and you're describing more tangible complications that they could see a rash or joint pain, swollen joints, then this is more obvious.
And I think what happens is that depression is deprioritized because you have a pressure maybe over a rheumatology visit, 15 minutes and they'll ask, review a symptoms question as to heart, lung, and kidney disease. And depression tends to be at the lower end of the hierarchy. And again, this is not because of any malicious or derelict things that are offered by physicians just goes under recognized. And the second thing that I talk about in the is a separate chapter in my book, devoted to Depression, is depression's not tantamount to sadness. So depression is a disease as complex as any syndrome. So depression hurts. Depression isn't just sadness, it causes you to withdraw from pleasures that you enjoy it. It forces you to [00:32:00] withdraw from family, friends, and and loved ones. So depression hurts, and depression causes fatigue. For example, depression causes cognitive impairment. So you have to dig a little bit deeper and not just say, am I sad? But I experiencing all these wire types of symptoms that can be associated with depression.
Leila: Definitely. And I think one last question that I have for this section of the interview is with Sjogren's disease, like with lupus and Ra, Sjogren's disease is a very common maybe second diagnosis that you may get afterwards. And I hear that Sjogren's has more neurological effects than maybe the maybe lupus and RA as well.
What are some of the very common neurological manifestations of Sjogren's specifically that we may, we may not see every day, but that say if you have RA and you're not even sure if you have Sjogren's, that may be kind [00:33:00] of like a. I, I, I may have Sjogren's if this happens, is there anything that you, that you can pinpoint?
Dr. Julius: Sure. So I, well it's the peripheral neuropathy, so like you're saying, patients with one autoimmune disease can have another autoimmune disease. So let's say you have both sjogren's disease and rheumatoid arthritis. If you start developing these small fiber neuropathies that are seen more prototypically in Sjogren's than at that point you would say, Hey, my neurological complications might stem from Sjogren's as opposed to rheumatoid arthritis.
Now, that's not to say that small fiber neuropathies can occur in rheumatoid arthritis, but probably at a much lower frequency. So knowing specifically the types and patterns of how neurological complications can occur in Sjogren's disease, when Sjogren's disease co-occur with another rheumatic disease, you'll have a better sense of understanding when I'm having a neurological disease due to [00:34:00] Sjogren's disease and when I'm having a neurological syndrome due to non sjogren's autoimmune diseases, which are occurences.
Leila: Got it. Yeah, I think the you just kind of put a light bulb in my head, especially like one thing that patients may also, have a mistake with is thinking that neurological symptoms just have to do with the brain as well. I think that's something that we, that may occur is that when you think of neurological symptoms, you're thinking about brain fog, you're thinking about dementia or Alzheimer's.
That's what neurological means to a lot of patients. So just like you said, remembering the nerve pain can be in any other part of your body, the peripheral side of the nerve sy nervous system. So knowing that just because it's not necessarily something happening in your brain doesn't mean that it's not a neurological symptom as well.
So just keeping that in you know, in in mind as well.
Dr. Julius: Right. And the last thing I'll say about this is that the neuropathies tend to be [00:35:00] undiagnosed in a lot of different rheumatic diseases. So for example, if you look at lupus, there's this nomenclature, ACR, the American College of Rheumatology nomenclature of different neurological symptoms.
And you could look at even the diagnostic criteria of lupus. So nowhere in the nomenclature of neurological lupus and nowhere in the diagnostic criteria of lupus is small fiber neuropathies talked about as well. So when we looked at neuropathies in lupus patients, the neuropathies were frequent and prevalent.
It was just under recognized. So I think this just emphasizes again that when we start our understanding how neurological disease and small fiber neuropathies that they're similar in different rheumatic diseases, although undiagnosed even lupus, that the neurological symptoms need to be revamped in understanding, and I would argue that the diagnostic [00:36:00] criteria and the ACR nomenclature of lupus needs to be greatly expanded and revised.
Leila: Absolutely. I think that that's a really good place to start with kind of, you know, the ACR is always the biggest place for all of our different rheumatologists to get the proper information and to get the proper naming and nomenclature, like you said, of the different symptoms and all of those things so that, that information and that, knowledge can be passed down onto their patients. And so I think that that's super important, like what you said. And thank you so much for giving us all of that information on the neurological manifestations of Lupus and Sjogren's. And I'm sure that there's so much more that we can even talk about and anybody that's super interested in learning more about these different topics.
Julius has a lot of other, a lot of other interviews and webinars and lectures that are coming up that we'll let you know about at the end of the episode. So stay tuned to learn more about that if you wanna hear more about these topics and all the places that you can [00:37:00] find them in the future.
And so, let's go into talking about the book and Julius's book is called Living Well with Autoimmune Diseases, a Rheumatologist Guide to taking charge of your health. And I think that this is such an amazing topic and, and book for a rheumatologist to come out with because you know, as patient organizations we always talk about empowerment, advocacy, making sure you advocate for yourself, but to hear it from a rheumatologist.
And to hear it from an expert that we should also take charge of our health. I think that that's super powerful and I thank you so much for bringing this to the table, and I'm so excited to hear a little bit more about your book and how this this project started for you and where you got your inspiration.
Dr. Julius: Yeah. Well, the, the, the title didn't come from myself. My, the title came from my wife and the cover, which has a which has a someone by the ocean who's running with a dog that, that came from my 9-year-old daughter, Samantha. So you always [00:38:00] have to look elsewhere for where you get original ideas. But the, the book, so the book is entitled, you know, like you said, living Well with Autoimmune Disease is a rheumatologist guide to taking charge of your health.
Now there are different features of this book, but the one thing I wanna emphasize as you're mentioning is that the core message of this book is empowerment, and I regard to this autoimmune empowerment. It's a unifying theme that occurs in all chapters of this book. So the book is relatively unique in that it offers a wealth of information about many different rheumatic diseases.
So the chapters on lupus, chapters on Sjogren's disease chapters on vasculitis, chapters on rheumatoid arthritis, chapters on psoriatic arthritis chapters on myositis and chapters on scleroderma. So it provides a one size fits all, so you could learn about these different rheumatic diseases. But the one reason that I wanted to juxtapose these chapters [00:39:00] is to emphasize that there is an inherent interconnectivity between these diseases.
So I think we talked about already how if you have one autoimmune disease, you could be affected by another autoimmune disease. But what's really fascinating also is that medications that initially were developed for one autoimmune disease is now being applicable to many other rheumatic diseases. So learning about these medications and how they're nimble andry and how they leap across diagnostic boundaries, I think is important.
I think when you're talking about these diseases, you know, family members often are affected by autoimmune diseases, not necessarily the same one. So, for example, if you have lupus, you might have a parent with lupus, but you might have a parent with Sjogren's disease or a parent with a rheumatoid arthritis.
So this offers you the opportunity to go to your family and say, Hey, here's a book that you might find are relevant. So that's the first feature of [00:40:00] the book is chapters on other rheumatic diseases. The, the second feature of this book is I intentionally wanted to put in this book that there are relevant features or issues that are not necessarily autoimmune in nature, but they have a big role in caring for patients with different rheumatic diseases.
So there are chapters on on fibromyalgia, there's chapters on diet, there's chapters on sleep, and I think these tend to be sometimes put in different books as if the diseases themselves and these non-inflammatory diseases are of lesser importance. But I did think that it's important to put chapters on fibromyalgia and on diet and depression in this book.
Finally, I think a third feature of the book that I think is really important to readers is that I wanted to open up my clinic, so I wanted to show readers the gripping drama that I'm privileged to see on an everyday basis. So I think that when readers read [00:41:00] about these narratives, what they happens is that in my patient's voices, they'll hear their own voices, and in my patient's struggles, they'll hear their own struggles. And what happened on, when you recognize this, you actually feel less lonely and and isolated, and you form bonds with patients you might not have otherwise met for the rest of your life.
So these are the features of this book. So I would say the unifying theme is autoimmune empowerment, and the first feature is the discussion on the different diseases in this book. The second is discussion on non autoimmune diseases that can occur in rheumatic diseases. And finally, third feature is using stories to help illustrate to readers and patients themselves how these diseases unfold in in time.
Leila: Absolutely. And I think two important things that you talked about in those features are one, here at AiArthritis, we [00:42:00] have a very unique grouping of autoimmune and autoinflammatory arthritis diseases. But the reason why those are grouped together is because we wanted, we knew that a lot of these patients have similar symptoms and wanted to be able to create a community of these patients that have similar similar similar things that occur in life, similar experiences, similar diagnostic journeys, just to feel that community, like you were saying, because these di these diagnoses and these diseases can be so isolating and. Feel like you can feel like you're the only one in the world that's experiencing something like this.
Sure. So I think that that's really cool that that's something that you acknowledge and something that's super important for us here at AiArthritis as well. And I think the second thing being that patients need to feel the empowerment of themselves to be able to take charge of their disease.
Like you said before, also, patients are gonna know their body the best. And [00:43:00] that's why we are also considered experts when it comes to our diseases because we're the expert in our body and the doctors are the experts in the medicine and the anatomy and all of the other amazing things that may, occur with these diseases, but there is always that one missing piece of your own personal experience that the doctor needs to be able to make the best assessment of what's going on at that time. So I think that those are such amazing themes for you to highlight in the book. Gotcha. And let's see.
Patients who get diagnosed with autoimmune diseases often feel really overwhelmed. And I, I'm sure that you may get that in your office all the time. I'm wondering if there's something specifically that you tell patients that are overwhelmed and, and maybe having such a hard time dealing with these heavy diagnoses.
Dr. Julius: So that's a great question and you can understand why patients feel overwhelmed because they might [00:44:00] come in with a certain set of symptoms. And the last thing they might hear is that the mosaic of these symptoms reflects an autoimmune disease. So what happens is the first question I get, well, can my autoimmune disease be cured?
And what I tell them quite honestly in the year 2025, is that autoimmune diseases can't be cured. So initially patients might be crest swollen or be pessimistic, but I say, hold on, hold on. So let's think about high blood pressure. So, high blood pressure is a chronic disease, it can't be cured, but it could be absolutely well managed.
High cholesterol, same thing, diabetes, there's no cure but if you take high cholesterol medications and medications that treat diabetes, you can still live a very long and gratifying life. And I think that's what happens very uncommonly, is that when patients hear that diseases can't be cured, they might hear that it can't be managed.
So there's a difference between cured and and managed. So I wanna [00:45:00] emphasize to readers and newly diagnosed patients that these are chronic diseases that can be very well managed, and that's the first thing. Then the second thing I tell them when it comes to autoimmune disease is you often hear the metaphor there's light at the end of the tunnel, but oftentimes I think we need to shift this thinking.
And there's also life at the beginning of the tunnel. And that's why when you diagnose someone with an autoimmune disease like rheumatoid arthritis, you might be discussing treatment at that very first diagnosis and you're discussing treatment potentially with medications that might not have been available more than 20 years ago.
So there's this burgeoning line of medications being approved year after year after year, and the options for you being treated are so much more than where it could have been 20 years ago. So. So that's where I try to tell my patients that there's light at the beginning of the tunnel. And if you hear that sense of hope [00:46:00] right at the time that you're diagnosed, I think that it makes these diseases a little less overwhelming.
Leila: Definitely. I think you, we talked a lot about metaphors this during this whole interview and during this talk, and I think metaphors are a really good way to talk to patients and to really get them to understand what we're trying to say. And I'd like the light at the beginning of the tunnel because there is, right. I, if you think of an actual tunnel, there's light at the beginning, there's light at the end. But if you also think about it, there's lights that are also in the middle of the tunnel as well. There's the lights that guide you through the tunnel, and I think that that's also a great metaphor for a chronic disease.
There's going to be lots of little lights and, and lots of little parts of darkness, and, and that's kind of the nature of the disease. But at the end of the day, there's still, there's going to be light. There's going to be times where you do feel good, there's gonna be good days, there's gonna be bad days.
So I really like that, that metaphor. I might steal that one from you. [00:47:00]
Dr. Julius: Thanks.
Leila: Alrighty. And I know that we talked a little bit about depression in, in the previous section. I know that with lupus, DD depression is listed as an actual symptom of the disease may not be that way for a lot of the other rheumatic diseases, although we know that it's something that occurs quite often. Is there any last bits about depression any little tidbits that you wanna share from the chapter of your book about depression?
Dr. Julius: Well, I think that recognizing depression right at the outset is really, really important. I. If depression goes by the wayside and it's percolates over many, many years, it can just remain something that is, think it's part of you, something that's immutable and can't be changed.
So I think, again, recognizing that depression can be managed and greatly improved, similar to any other, what we call organic complications. So depression can be treated in much the same way that joint and skin disease can be treated. So I [00:48:00] think recognizing depression as occurring early on can have a gratifying response to treatment and then it could grant you a sense of optimism and resilience.
So the whole way in Lupus is affecting you can be managed with a lot more hope.
Leila: Absolutely. And like you said, noticing it as a chronic disease as well, that can be treated, that can be you know, there can be interventions for that and not thinking that it's something wrong with you, which I think is what a lot of people may discount depression as, but you have to really realize that it is a disease. But yeah, definitely seeing depression as, as a full on disease. It's not just, you know, something that's going on in your head, but something that can be treated and should be treated for you to be treated as a, a holistic person that has this chronic illness.
So, I think that that's really important for patients to also feel empowered about. Okay. I think that this [00:49:00] comes to the end of our interview. I have one last question. You talked about the three features of your book, but what is the biggest takeaway that you want patients to get from this book?
And give us a few reasons why they should go out and, and get the book.
Dr. Julius: Well, I think the biggest takeaway in this book is that like we talked about, we talked about diseases, we talked about diseases that impact such as fibromyalgia. We talked about stories, but at the end of the day, what I wanna emphasize again is that readers should feel empowered, and again, autoimmune empowerment.
So I really think that different strategies I use in the book that when you walk away from this book, I think that it can be a transformative experience and just that sense of empowerment. That sense of owning your disease and knowing that you can make important changes, that sense of empowerment is something that I wanna be the parting message of this book.
Leila: Amazing. I think that that [00:50:00] is so so powerful for patients to know coming from a rheumatologist. And yeah, thank you so much for being here today and for sharing about your book and for the information about the neurological side of Sjogren's and lupus. I think that that's, this information will.
Really help a lot of patients to understand what may be going on with them if they were not sure if this pain that they're feeling was something that is related to their lupus or Sjogren's disease. So I thank you so much for that and Sure. Yes. Please let us know what's coming up next for you and where we can find your book.
Dr. Julius: If you wanna learn about my book a little bit more and where it could be bought, you could look at juliusbirnbaum.com on the website, and it could be purchased at Target. It could be churches that Barnes and Nobles and could be purchased on the Amazon websites.
Leila: Awesome. So anywhere that you can find books, you can probably find this book.
Again, [00:51:00] the title is Living Well With Autoimmune Diseases, A Rheumatologist Guide to Taking Charge of Your Health. And like we said, you can go check out juliusbirnbaum.com. There's information about the different shows and podcasts that he's been on as well as some upcoming and we wanted to highlight a few of the different webinars and lectures that he's gonna be having with other patient organizations that are amazing partners of ours as well.
So we wanna make sure that we champion all of the work of our partners. So a few of them are on April 8th at 6:45 PM Eastern, there's a lupus and you segment that's gonna be about lupus and pain management. Julius is gonna be talking about fatigue, and that's with lupus Foundation of America.
The on the 24th of April, he will be talking about inflammatory arthritis, a guide to medications, lab tests, and management of side effects with the Arthritis Foundation with the Association of Women in Rheumatology. He'll be talking about Sjogren's and [00:52:00] neurological complications that's coming up in the next few months, as well as a series of different talks with the Autoimmune Association having to do with introduction to Dr. Birnbaum's bio discussions about multiple different autoimmune diseases, depression and patient empowerment which are all, you know, super important topics as well. Lastly is an interview with AARP about psoriatic arthritis. So for all of you listening to the AiArthritis Voices 360 Talk show I'm sure that one of those
talks will be interesting for you to take a look at and to get some more information on. And I wanted to talk a little bit about what AiArthritis has in in the funnel right now as well. What's coming up for AiArthritis? As all of you may know if you are a recurring audience member on May 20th, we have world Autoimmune and Autoinflammatory Arthritis day, and there's always lots of activities [00:53:00] that come up with that. So make sure to stay tuned for more information about our social media campaign and livestream that will be going on the week of May 20th. This year we also are going to, we have a, a fundraiser that you can create your own race team.
So if you go to give butter, givebutter.com/AiArthritisDay25, you can either donate or you can start your own race team to be able to get donations for AiArthritis, for this world AiArthritis Day. And as you all know, we do an auto theme for this, for this awareness state. So we are excited to see all the different car puns that you have describing your disease or your symptoms to those of a car.
You know, maybe you know your rheumatologist is the mechanic and is helping you tune up your car. Let us know all those different fun car puns that you may have. And post 'em on social media, on [00:54:00] World Air Arthritis Day on May 20th. And you can use the #AiArthritisDay and #LearnArthritis
to be able to elevate your social media posts so that the whole community can see it. And yeah, that is what we have in our funnel. So at AiArthritis, we don't just represent the patient voice. We are the patient voice. And with your support, we can amplify it even further. If you found value in this talk show, consider making a donation to help us continue pro producing impactful conversations, bringing all stakeholders to the table to discuss patient identified issues and patient infuse solutions. Visit AiArthritis.org/donate to help make a difference together. Thank you again for tuning into this episode of AiArthritis Voices 360. You can find AiArthritis on all major social media platforms at. IF AiArthritis. And that's a wrap.
We will see you [00:55:00] next month for the next episode of AiArthritis Voices 360. Thank you again to Dr. Julius Burnbaum for being such an amazing guest here on the show. All righty. Bye everybody.
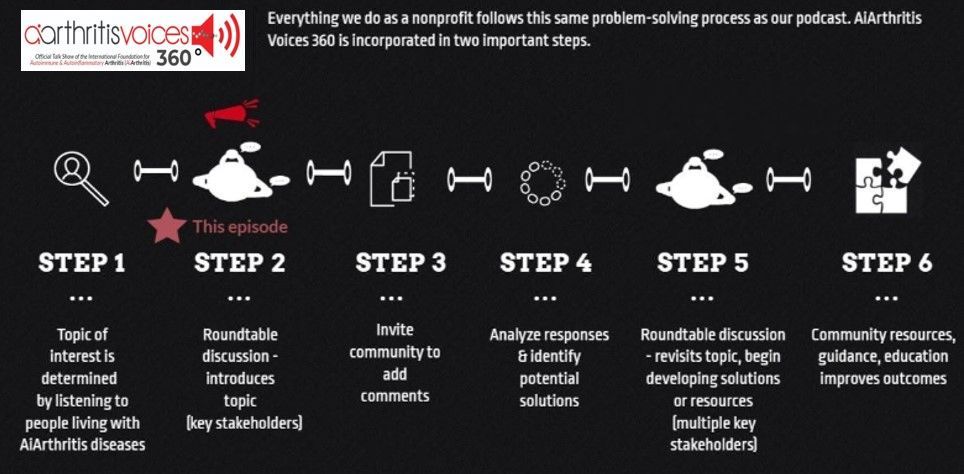
All our main 1st Sunday of the month episodes are either an initial "put the topic on the table" episode (Step 2 in our organization's 6-step problem solving process) or a "revisit to the table" episode (Step 6 in our organization's 6-step process), where we build on a past show because we have moved forward in developing help, tools, or projects around the issue (Step 5 in our organization's 6-step process).
After each show airs we spin off the conversation into many discussions over various formats, which we now call #360its.
-
Additional Resources & Information
- Learn more about Lupus
- Learn more about Sjögren's Disease
- Volunteer with AiArthritis
Your Host: Who is at the Table this Episode?
Leila P.L. Valete, Health Education Manager
Leila P.L. Valete
is the Health Education Manager at the International Foundation for AiArthritis. She is a person living with Lupus & Sjögren's. She is passionate about inclusion and diversity in health education and meeting individuals where they are at in order to learn in a way that resonates with them. Leila is on social media as @Lupus.Lifestyle.Lei sharing bits and pieces about her life with lupus and connecting with others.
Dr. Julius Birnbaum, Rheumatologist, Neurologist, Author
Dr. Julius Birnbaum
is a distinguished rheumatologist with 20 years of experience and the only physician in the U.S. trained as an internist, neurologist, and rheumatologist. He completed his medical training at Columbia, Mount Sinai, Jacobi Medical Center, and Johns Hopkins, where he later pioneered a Neuro-Rheumatology Clinic to treat complex neurological complications of autoimmune diseases. Dr. Birnbaum has authored over 30 publications in prestigious medical journals and has been a featured speaker at national and international rheumatology conferences. Currently, he serves as Associate Professor of Rheumatology at the University of Pittsburgh Medical Center (UPMC) and Division Chief of Rheumatology at UPMC Mercy Hospital, where he continues to teach and mentor medical trainees. Outside of medicine, he enjoys sports like basketball, swimming, and running, which he shares with his wife and three children in Wexford, Pennsylvania.
Pull up your seat at the table
Now it's YOUR TURN to join the conversation!
What do you think about this episode?
We want to know what you think! By continuing the conversation with your opinions and perspectives - we all get a better understanding of the problems facing our community. Better yet, through these conversations we can start working and developing solutions.
We mean it when say 360. Not only do we want your input anytime and anywhere, but we also are eager to see where the conversation will take us. So please, "pull up a seat at the table" and let's start talking!
Email us at podcast@aiarthritis.org, message us on social media (find us by searching for @IFAiArthritis)
Relevant Episodes & Projects
Ep. 98: Mental Health & AiArthritis Diseases
As more treatment options are moving towards Biosimilars, many questions are being raised by patients. What are Biosimilars? Are they safe and effective? Are there downsides? Upsides? What are doctors' opinions on Biosimilars? What should I do if I am switched to a Biosimilar?
Ep. 105: Breaking Research at ACR 2024
Do biomarkers hold the key to understanding disease severity and predicting disease onset? Tiffany and Patrice discuss the importance of biomarkers & their uses for disease treatment.
Ep. 101 "Go With Us!" to EULAR 2024
Join TIffany and Rick as they address the challenges involved as Treat 2 Target has emerged from aggressive treatments for a larger population to treating per the individual and based on the complexity of each disease.
Ep. 18 The Juggling Act: Living with Multiple Conditions
Info here about puppies being awesome
Love the show? Help us make sure we stay on the air by making a donation.
Your contribution helps us continue the work we do every day to improve the lives of millions worldwide.