Elevating the Patient Voice
AiArthritis Voices 360, Episode 103
Air Date: November 3 , 2024
This episode is a Step5, as outlined in our 6 Step Patient-Led Problem Solving Process.
In this episode of
AiArthritis Voices 360, co-hosts Leila P.L. Valete and Brittany Murray—both living with AiArthritis diseases—dive into the power of patient voices in transforming the healthcare experience for the AiArthritis community. They bring empathy and validation to stories submitted by listeners, highlighting real struggles with insurance, pharmacy issues, and the emotional toll of chronic illness. Brittany also shares key takeaways from the recent Autoimmune Community Summit, covering practical tips for self-management, understanding the influence of environmental factors, and the importance of owning and sharing your story to drive change.
This episode is packed with relatable stories, actionable advice, and encouragement for anyone navigating autoimmune challenges. Tune in for new ways to elevate your voice and join a supportive community that understands.
Episode Highlights:
- Leila and Brittany discuss the impact of elevating patient voices in the AiArthritis community.
- Patient-submitted stories reveal real challenges with insurance, pharmacy issues, and living with chronic illness.
- Key insights from the Autoimmune Community Summit highlight the importance of self-management and environmental factors.
- Tips on using personal stories in healthcare advocacy help patients drive meaningful change.
- AiArthritis’s "WTHellth" project aims to address systemic barriers in healthcare.
- The hosts share tools like communication aids and advocacy programs for patient empowerment.
AiArthritis Voices 360 is produced by the International Foundation for Autoimmune and Autoinflammatory Arthritis. Visit us on the web at
www.aiarthritis.org/talkshow. Find us on Twitter, Instagram, TikTok, or Facebook (@IFAiArthritis) or email us (podcast@aiarthritis.org). Be sure to check out our top-rated show on
Feedspot!
-
Expand to View the Podcast Transcript
[00:00:00] Intro: Welcome to AiArthritis Voices 360, the podcast solving today's most pressing issues in the AiArthritis community. We invite you all to the table where together we face the daily challenges of autoimmune and autoinflammatory arthritis. Join our fellow patient co hosts as they lead discussions in the patient community, as well as consult with stakeholders worldwide to solve the problems that matter most, whether you are a loved one, a professional working in the field, or a person diagnosed with an AiArthritis disease, this podcast is for you. So pull up a chair and take a seat at the table.
[00:00:47] Leila: Welcome to AiArthritis Voices 360. This is the official talk show for the International Foundation for Autoimmune and Autoinflammatory Arthritis, or AiArthritis for short. My name is Leila P.L. Valete and I am one of your co-hosts today. I am a person living with lupus and Sjogren's Disease, and I am the health education manager here at AiArthritis, and I am joined by my co-host and rockstar AiArthritis volunteer, Brittany Murray.
So Brittany, if you can go ahead and tell everybody a little bit about you.
[00:01:17] Brittany: Sure, I'm Brittany Murray. I'm a patient living with psoriatic disease, among other chronic diseases. I started volunteering with AiArthritis almost two years ago, and I have a small blog called Chronic Disease Diary where I go to vets.
[00:01:34] Leila: Yeah, we've really enjoyed having Brittany here for the past almost two years. She's been able to jump in and help us with some data stuff, some video stuff, a lot of different things that we've been needing help with. So I wanted to give Brittany a little bit of a round of applause and thank you for all the help that she's done with AiArthritis.
And one of the segments today is actually designed and put together by Brittany. So we'll talk about that. But our topic today will be elevating the patient voice, which at AiArthritis, we do quite often, but this is a talk show episode directed specifically for that, because our first section that we will be having is our rant section.
And our rant program is one of our most highly regarded programs here at AiArthritis, because everybody has something that they're a little angry or frustrated about when it comes to AiArthritis diseases. So we love to make sure that we give patients a platform to be able to say what they need to say, because we all know how frustrating it can be with these diseases.
And so with these rants, we take patient identified issues and create patient infused solutions. So a few of our different programs have come from specific rants that we've had that people are seeing, you know, the different issues that they have with their AiArthritis disease. And we've had projects and programs come to help and mitigate those issues.
And so that's our first segment. We'll be talking about rants and reacting to a few rants that we have here. And then we will also have our second segment, which Brittany has prepared for us. So if you want to give just a little preview about what we'll be talking about.
[00:03:15] Brittany: Yeah. So last week, the autoimmune association had their annual community summit and they brought researchers and entrepreneurs and patients from all around the world to give us the latest on what's happening in the autoimmune community research and clinical trials and tips and tricks that we can use.
So we're going to go over some key takeaways from that summit.
[00:03:37] Leila: Awesome. And yes, thank you to the autoimmune association for putting together such an amazing summit. This is the third one that I've been able to attend and we had a virtual booth there. And so I'm excited to reach out to all of those who stopped at our booth.
So, but thank you again to the autoimmune association for holding a free educational summit for all patients to be able to attend. It's really important that these. types of educational summits are accessible to patients. So making it free is the best way to be able to do so. So I know, you know, speaking for a lot of patients that we really appreciate that so that we're able to learn as much as we want to with these different summits.
So that is amazing. Alrighty, so let's go ahead and jump into this first rant. I'm going to go ahead and read it and then we'll give some commentary. Some of these people did allow us to use their first name, so we will credit them for their rant with their first name. Others asked to stay anonymous, so you will also see that.
And if you are one of the people who you hear your rant here, go ahead and comment down below, either on YouTube, if you see this on Instagram As a clip, let us know that this is your rant. And if you have a rant that you want to submit, you can go to aiarthritis. org slash rant to go ahead and submit something.
So let's go ahead. So this first one is specialty pharmacy billing. I feel like we will both understand about this one. Definitely. Okay gave them all the information regarding my Arentia co pay assistance. First order, they hit my debit card for my co pay, called them and explained I don't have a co pay for Prudent RX.
Next order, they hit my debit card, this time for the whole amount of $1745. Called my case manager through insurance to help resolve this. We spent one hour on the phone talking to Arentia co pay assistance rep, Prudent RX rep, and the CVS specialty pharmacy rep. How hard is it to verify the information I've given you many times?
I've even made copies of the paperwork and mailed it to them. I had to report my debit card loss so they can't hit my bank account. Now that they have it straightened out, so where is my $1,945 that you took out of my bank account? I hate having to do the legwork and them having to do their jobs too. Oh my goodness.
Any initial thoughts first?
[00:06:01] Brittany: I think it's happened to all of us at this point. And like how Not only do you have to worry about if your card is on your prescription pharmacy account, but you also have to worry about, well, if you use them for this drug and you are supposed to get charged but you don't use them for this one, that you shouldn't, and trying to manage that on top of them trying to manage that is just anxiety inducing.
[00:06:25] Leila: No, definitely. And it like when you're talking about $1,700, like we're not talking about $100, $200 here, but even for some patients, $200 would break the bank. So this is just, oh man, this like really pisses me off, to be honest like, I really don't put my, if I cannot all avoid it, I won't put my payment information because I know that I'm not supposed to pay, so I don't want them to accidentally charge me.
But. I didn't even think about it. Like what you said, like with, if you have multiple medications going on, you can't even avoid it.
[00:06:55] Brittany: Yeah. Yeah. I'll never forget. I think the first time it happened to me, I was sitting outside like Target in the parking lot on hold talking to one of the pharmacies, then talking to the co pay assistance program and then talking to another program my employer provides and just running them all through the same information over and over again and they'll be like, Oh, this should never happen.
Always call us. And it's like, but I don't have eight hours to sit and talk to you, you know? Every day.
[00:07:23] Leila: I mean, and by the way, this was a rant from Cindy. So thank you, Cindy, for giving us your rant. This is actually another project that both me and Britt have been talking about recently is our WTHellth project.
And this has to do with rants specifically about insurance situations about pharmacy pricing and all of this stuff. So I actually know who Cindy is. So maybe I'll see if she'd want to submit this rant to WTHellth, because this is a serious #WTHellth situation like seven, 19, she's out $1,900.
Seriously. WTHellth. So, I'll tie a little bit more information about that, WTHellth program as well, we will have an informational blog coming out in the next week talking about that. So it'll be super interesting. So if any of you guys have specific grants that have to do with insurance, pricing, anything like that about drug affordability, all of that, please feel free to go ahead and submit those rants to www.aiarthritis.org/rant so that we can get those specific stories for all of our WTHellth videos because we are pushing back against PBMs and all of the different drug affordability boards that are coming up because it is causing hell for patients pretty much. That's why it's called WTHellth
So, I had to do that little plug there because I don't know if another insurance one is coming up, but I wanted to make sure that we did that. Alrighty, let's go for rant number two, The Cycle of Never Getting Better. Ugh just the title gets me sad already.
[00:08:58] Brittany: Haha.
[00:08:59] Leila: It's so frustrating as I sit here getting ready to clock into work for a job that is slowly making my condition worse because of the stress of the job.
But yet, I can't leave this job because I need good health insurance to cover my appointments, labs, and meds, or that I can't reduce my hours because I can't afford to live on a part time income. Definitely something that I've thought about before and in previous jobs that I've been in I stressed myself out all the way into lupus nephritis and I had no idea that it was killing my kidneys as I was just because I was so stressed.
So, oh man. This is such a hard cycle that we live through, and just acknowledging it sometimes is really sad.
[00:09:43] Brittany: It really is. And if you don't have another job that you can go get, not that the job market is ever easy, but then you're really stuck. I know I switched jobs once, not for many reasons, but one of them was I got a migraine every Friday like clockwork.
And I was like, okay. So at the end of every week, I'm so stressed out that my body freaks out and I get a migraine and then I'm fatigued. And then you end up in that cycle again. And it's unreal. And I was lucky to be able to find another job. But of course I waited, you know, after months and months of having weekly migraines.
[00:10:17] Leila: Yeah it's very hard because I even had an employer before tell me, no one else is going to want to deal with your health issues like, he wasn't my employer wasn't even letting me go to the doctor as much as I needed to. And he had the audacity to gaslight me and say, well, no one's going to want to deal with your health issues anyway.
So you might as well just stay here cause I'm the only one that'll, you know, that'll really, you know, take you on. And I'm like, okay, that's the issue.
[00:10:43] Brittany: Yeah. There are things to protect you from that. Yeah. And there are laws.
[00:10:50] Leila: When you're just straight out of college, I really, I was like, I think I just really let this guy gaslight me for no reason.
[00:10:56] Brittany: Yeah, definitely. And it's so taboo too, to be like, I need to go to the doctor. I need FMLA. I need disability. And it just makes it even harder to go get.
[00:11:07] Leila: Yeah. And I totally do advocate though, for if you can, at least survive on the 60 percent and you really do need a break. Taking disability, if it's two weeks, if it's a month it's a really pain in the butt to go through the actual process of it, but sometimes your body just needs it.
And if you have the ability to do so, not talking about like your workload or any of those kinds of things. If you work full time and you can afford it and you can still live off of that 60 percent for a month or so, I would, I still highly advocate to use the disability that you are offered if possible.
Alrighty, let's do it. Rant number three. Inappropriate treatment. One morning, I woke up feeling severe pain in my finger, joints, wrists, and ankles. Oh, finger joints. Finger joints, wrists, and ankles. I had difficulty moving my hands and legs, so a relative helped me go to the hospital. However, the neurologist I initially saw didn't know the cause of the pain and referred me to a physician.
The physician prescribed me painkillers without diagnosing the disease or explaining anything to me. It brought temporary relief. But the pain returned after almost a year. While working at a rehabilitation center, my colleagues, who knew about rheumatoid arthritis, suggested that I get a blood test for RA, which came back positive.
In 1999, regrettably, the country lacked the presence of rheumatologists. Thus, I was once again prescribed pain relief medication by a general physician. Oh, man, that is really tough. Yeah. And he, you know, this person, Prakash, who submitted this rant, he, oh, there's more to the story. That's why I didn't see it.
Hold on. Pause for a dramatic effect. I was taking painkillers and somehow managing my pain and moving. In 2007, I came to know there was a rheumatology clinic in Kathmandu. I booked an appointment for a consultation with a rheumatologist. The clinic was very crowded. Patients from all over the country had come for treatment.
I waited for a long time for my turn, but the doctor only spent one minute with me. He asked me a few questions, suggested some tests, and prescribed more painkillers. The tests were very expensive and hard to pay for by poor people from rural villages. I did not like the behavior of the doctor and the staff of the clinic.
No counseling is offered and patients are not provided with information about the disease or what they can expect from treatment. Took me almost 30 years to get appropriate advice and treatment from a qualified rheumatologist. Thousands of people are unaware of the disease and treatment for any arthritic conditions.
Because of expensive tests and treatment, many people are not going for treatment. It's said they're using herbal medicines, which may increase the risk of worsening the condition. People in need are left to suffer due to the lack of support and treatment provided by the government healthcare system.
Man, that is, you know, I think like just in general with any foreign countries, like sometimes as Americans, we're just like blind to how their system is and how people in other countries are also even more so suffering because of the lack of advancements in those countries. So it's really sad to hear that it took 30 years for him to actually get appropriate treatment.
Yeah.
[00:14:35] Brittany: Yeah, and that the treatment is not something that's going to reverse or prevent damage. It's just going to give short term relief and possibly cause other problems.
[00:14:44] Leila: Yeah, exactly. I mean, and what he was saying too is that basically when they got the tests, like, how do you pay for those tests if there's not any insurance system that's put together or anything like that?
And I had to look back real quick to see where he's from, but he's from Nepal. So it's a smaller Asian country, and I'm sure that they don't have, you know, took a little bit for them to get the advancements in treatment. And so that's really unfortunate, but it is also good for us to know that these things are still happening in other countries.
So even, you know, just spreading awareness and just trying to see how many, you know, how many more people we can even get from that country so that we know what's going on is super important as an international foundation. So yeah, definitely. Thank you so much, Prakash, for sending us this story, and I really do hope that, you know, in the future, it will improve and that even now, so hopefully people who are just getting diagnosed are getting treatment, you know, a lot faster than what you did, but it doesn't negate, you know, the 30 years of suffering that you had up until then.
So I'm really sorry for that. Alrighty, number five, don't interfere with the physician patient relationship. Government, though it is specifically illegal, has done a great disservice to the chronic pain patient population, of which many AiArthritis members associate themselves by permitting the CDC and local state governments to create data and fact deficient guidelines for physicians who prescribe opiate and opioid medications, the gold standard treatment for arthritis pain historically.
I am having a little bit of a hard time comprehending this one. So she's saying that They're creating guidelines for physicians who prescribe opiate and opioid medications. So maybe it became more regulated, like the
[00:16:42] Brittany: Yeah, I'm wondering if it's harder to find or harder to get the medication that you need, knowing it's like one of the only things that has helped you.
[00:16:49] Leila: I have seen a little bit more of like the pharmacies that I go to, there's specific medications that they say that they don't fill anymore. Some of them being opioids, one of them also being What's the what? Promethazine or, you know, those kinds of cough drugs as well too. So yeah, maybe in some states it's just becoming a little bit more difficult to prescribe those medications that a lot of, especially a lot of patients that were diagnosed like a while ago, a long time ago, where they have a lot more damage.
A lot of them are only really surviving off of pain medication to get through the day. So that's really tough.
[00:17:27] Brittany: Yeah, it's increasing risk of having to look for other ways to either get your medication or find other like off the market treatments or herbal treatments, you know, therapies.
[00:17:40] Leila: Yeah, that's actually the one thing that I wanted to comment from Prakash is I forgot to mention this, but he said that, you know, so many people are choosing to try to find herbal supplements.
And that's one thing that I want to highlight this. Also, if we can make this a clip, I really want to make this one a clip, but specifically that herbal treatments, a lot of them, when you look at them, when you say you have an autoimmune disease or you have a deficiency in your immune system, a lot of people will want to take the ones that say they boost your immune system.
And it does the absolute opposite of what it needs to. It is boosting your immune system to attack your body even more. What we need as autoimmune patients is immune suppressants, not immune boosters. This is the most important thing to remember, is that supplements like ashwagandha and other ones that are super popular right now please, for everybody who has an autoimmune disease, do not take anything, unless, you know, certified by your doctor as a, you know, a good source of a supplement, do not off the market take anything that says it's going to boost your immune system because it can actually cause you to flare if it boosts it enough.
[00:18:56] Brittany: And it's hard to know because everyone pushes that stuff for you and there's little Instagram ads and stuff that say take this if you've got an autoimmune disease and then you go and Google like, Ooh, is this going to interact with my medications?
Like do not take and you're like, Oh, okay.
[00:19:10] Leila: Yeah, immune support, you know, all of those things. Yeah, they can be counterproductive. So just be really cautious of that. Okay, I think this is going to be the last one. And then. Maybe we'll have another episode of these with the rest of the rants that we have.
Again, if you have any rants that you want to submit, www.aiarthritis.org/rant. And we would love to be able to read your rant on the next talk show that we do of these. So let's go to our seventh and last one. Sick and tired of being sick and tired. I just want to wake up pain, fatigue, and ache free.
I'm tired of the blank expressions on people's faces when I am in a flare up, or even not in one, when I tell them ankylosing spondylitis affects just about everything in my body, and basically controls my life. Oh, you should do Pilates, yoga, and pray more. It helps. Be grateful to be alive. Stay positive.
Look at the bright side of life. You should use this oil and drink this mixture. It cured my second cousin on my grandma's big toe side of the family from cancer. You don't look too sick. You are too young. You look fine. And you did this the other day. Yesterday, I cannot stand my body not operating fully.
My mind feels like jello. Last thing I want to deal with is unsolicited advice. from someone who can hardly handle a normal headache. I am tired, drained, and frustrated with myself and my situation. I took on a new role career wise and I regret it. I'm overwhelmed and wish I didn't need the income to afford my treatments.
This sucks big time. Ain't that the truth? Man, she was
[00:20:56] Brittany: I feel that.
[00:20:59] Leila: And both of us were actually diagnosed very young, right? You, how old were you when you were diagnosed?
[00:21:04] Brittany: Two.
[00:21:05] Leila: Wow. How old? Yeah, way even younger than how old I was. And that was with psoriasis.
[00:21:11] Brittany: Yeah, psoriasis and arthritis, like officially as a teenager.
Yeah.
[00:21:16] Leila: Yeah. And so I was diagnosed officially with lupus at 12, but I had ITP, which is another autoimmune disease when I was eight. So basically, Since I was eight, I've been dealing with autoimmune diseases. So the you're too young situation is the, it's still crazy to me that people will still say that.
[00:21:37] Brittany: Yeah. Oh, yeah. Every day. Every day someone's like, I can't believe that you'd have arthritis only old people get that or you shouldn't be that tired. Well, okay. Well, yeah.
[00:21:48] Leila: Yeah, I literally am. So I don't know what to tell you. You're like you, you're you tell my body that because I've tried to tell it for the past 30 years. So I don't know.
[00:21:58] Brittany: Yeah, I, we're going to touch on some of this stuff in the summit summary and like all these things will help you. Like if you do yoga, you're active, you pray more, all those things can help you and contribute to your wellbeing. But also if you're tired, your body is telling you to rest. So do it, you know, let yourself and it's so hard to do, especially with an autoimmune disease.
If you are tired every day. You obviously can't live your whole life by resting. So trying to find that balance is so hard, but please take a break.
[00:22:30] Leila: Yeah, no, it's really hard to find the balance, but I can say that I definitely once I started working out again, like lifting weights, doing yoga and Pilates specifically to those did really help my energy and my pain.
So it really is on a, person by person basis and people, you know, they do have the best intentions, but sometimes it's just better to just sympathize with someone that's what, or empathize and sympathize with someone, you know, advice isn't always needed. You can just say, you know, that really sucks.
And I think someone would genuinely like feel better and feel like, hey, they kind of understand what's going on rather than, you know, maybe trying to give some unsolicited advice. And I think I need to take that advice as well. Like, I feel like I'm always trying to give people advice. So yeah, maybe, yeah, maybe sometimes we just say, yeah, life sucks and I'm sorry you have to go through that and that might make them feel better. So I think that was a good one to end on. And yeah, let's go ahead and jump into the next segment and see what we have to learn.
[00:23:34] Brittany: Right, so, as we mentioned earlier, last week was the autoimmune community summit, and as Leila said, it's free. I saw they put the videos on YouTube a couple of months after the summit, so watch out for those.
Check out the blog because we sum it all up there, but we just have a few key takeaways, actually four, that we're going to really focus on as themes that were covered during the summit. So, the first one is owning your story. And I think at AiArthritis, we talk about this a lot. The patient's story is everything.
We know how we feel. We know what we've experienced. We know what the disease is really like to live with every day. And even our doctors don't know that. So you have to own your story. You have to know what it is. You have to share it. Even if it's just with yourself or your doctor, you got to share it. So one of the keynotes talked about some tips that you could do to get started in sharing your story. And that is really to know why you want to share your story. What are you trying to get out of sharing your story? Who are you going to tell it to? Are you going to tell your mom? Are you going to tell your doctor?
Are you going to post it on Instagram for everyone to see, kind of know your audience? And know how you want to deliver it. How do you want people to receive your story when you share it? And that can really help you design how you want to share your story and kind of get the right message out. But as I mentioned, you can share it with your doctor and you should share it with your doctor.
They need to know what you're experiencing, how you're feeling, what your values are, and what you want to get out of your treatment right now. Having that dialogue gives your doctor the information they need to collaborate with you and partner with you on your treatment plans and what services they might offer to you.
And without that, they're guessing based on data, you know, and what little you provide. So share with them what's really happening with you. And if you have trouble connecting with your doctor, maybe they aren't hearing you or they're not collaborating in the way that you really need to. If you're comfortable with it, tell them that.
Tell them that you're not feeling heard or that you feel like you're not getting the right treatment path. And if you're not comfortable with that or you have the option, go find another doctor. There is somebody out there that will listen to you even if it's not a rheumatologist and that's what you really need.
Find a doctor that will listen to you if it's your primary care and get a referral to somebody that will listen to you. There's so many ways.
[00:26:00] Leila: Just to jump in here a little bit, like definitely telling your doctor your story is super important, making sure that you can communicate with them. One of the things that we do here at AiArthritis is also help with the doctor and patient communication barriers that there may be.
If you want to check out, we have a few different episodes of our RheumyRounds segment here
where we talk about doctor patient communication and we get the doctor's side of how communication goes and the possibilities of what could be going on when you have these doctors appointments, we get to hear like, yeah, the doctor is running around trying to see 60 patients in a week. And how is that even possible? So having empathy and sympathy on both sides is important.
We also do have communication aids that we will be premier. Well, it is premiered. We have the JIA communication aids where it's an appointment guide that we can really help with the different conversations that might happen at your rheumatologist's office. And so we have that guide. We also have a clinical trial decision making aid that can help with any of those communications specifically about clinical trials as well.
So we do have some different tools here at AiArthritis and we are planning on that JIA appointment plan to be able to expand it to all of our different diseases as well into adults. So if you want to check that out, you can see it at AiArthritis.org/JIA communication and you'll be able to check out what that appointment plan and you can go ahead and print it out still and use it for yourself and just, you know, cross out the stuff that has to do with being a JIA patient, specifically a kid, but all the other tracking situations is good for anybody of any age. So just wanted to let you all know that we do have some tools to help with the communication as well. And also telling your story. Are you part of AI Advocates Brit? Yeah. Yeah. We should talk a little bit about AI Advocates and what that program is a little bit to help tell your story as well.
[00:28:06] Brittany: Yeah, so that program is super cool, and I'm really new to it, but if you've shared your story once, you can share it again, and AiArthritis and other organizations have training to help you get better. One of the most impactful ways that you can share your story is by talking to your state representatives, or the Center for Medicaid, or other organizations to really share how the patient experience impacts some of the decisions that they're making. They might be saying, well, we don't need this drug anymore. And you're like, but that's the only one out of 20 that have worked for me, you know, and really sharing that with them and how it impacted you can make all the difference in the world and even change a law.
So if you are interested in getting in that program, we want you here.
[00:28:50] Leila: Yes, absolutely. So you can go to AiArthritis.org/advocacy and you can learn more there. So thank you. Sorry, that was a long blurb, but telling your story is such a huge thing. So I wanted to make sure that everybody is able to get the resources that they need.
[00:29:06] Brittany: Yeah, it's so important. So one of the other things that we're going to talk about is the genes aren't everything, and I think we've been programmed as autoimmune patients, it's like, it's in your genes, it's your whole body, it's everything. That's why you have this disease and there's nothing you can do about it.
Like, okay, now what? So one of the things that they covered in this is genes aren't all of it. They're actually maybe like 10 to 30% of what is triggering and causing our diseases to exist and progress, so it's been pretty evident that we need to pay attention more to our environment, whether it's climate change or childhood trauma or your diet, they all contribute to when and how your disease is presented.
Research has been showing that autoimmune disease has been on the rise for the last 40 years, and nothing has changed more than the environment. So you might be thinking like, Oh, climate change has nothing to do with it. Well, let me tell you how it does, because I was amazed. So one of the examples is air pollution has decreased the protections of the ozone layer.
And I think we've been hearing a lot about air pollution has been increasing because of manufacturing and cars and all the other things that we have. But that decrease in the protection from the ozone layer exposes us more to UVB, which actually increases our risk of developing lupus. Another example is the American diet. Highly processed foods, lots of animal products. Both of which are tied to inflammation. Inflammation is a key contributor to autoimmune disease. Another example is if you have two adverse childhood experiences, or what's called ACEs, you increase your risk of developing autoimmune diseases. Of course, you're a child, you can't really control a lot of what's happening, but it's important to note that those childhood traumas do make a difference in your life, or in your kid's life if you're a parent.
So, if you lose a parent, or a sibling, or you've been exposed to domestic violence, or maybe, like me, you were prematurely born. Those things contribute to your likelihood of developing an autoimmune disease or triggering one that's there already. And of course, there's even smaller things like an infection.
You get a common psoriasis trigger. You could get a cold and cause your immune system to flare. So the genes you have make the disease possible, but those environmental triggers activate the disease and drive the disease progression.
[00:31:29] Leila: Yeah, I can't tell you even more that all every single flare that I've had and every single onset of any autoimmune disease that I've had have all been from viral infections.
I have like, I didn't connect the pieces of that until maybe about a year ago. And then I went back and figured out every single time that I've had a huge flare has been from a viral infection or something like that happened.
[00:31:51] Brittany: Really?
[00:31:52] Leila: Yeah. So that is wild. Wild. And one other thing is I, you know, I think a lot of people do have adverse childhood experiences, whatever it may be, you know, it may be that, you know, your family didn't have enough money to provide you with, you know, meals at school.
And so, you know, that's kind of a trigger for you or any, anything that could cause some kind of childhood adverse events. With that I can't recommend therapy enough, you know, some therapy may not be, you know, good for some people, but, you know, there's different types of therapies that you can try. It's not just talk therapy.
There's a lot of other options out there. Starting out even with a support group having to do with your disease could be a good way to start. But I cannot tell you that ever since how much I've healed of some of my childhood trauma, how much better my lupus has been since I've been at peace with that. So take with that what you will.
It could be placebo. It could be, you know, I was taking therapy and now I have a better job. So I have enough money to take care of myself more. It could be a correlation rather than a causation. But I think addressing those inner work. It can help with a lot of things, not just your autoimmune disease, but relationships and all of those types of things.
So if therapy is something you're open to, it's never too late to try.
[00:33:12] Brittany: Yeah, and there was an example that they gave during one of the summit sessions where they actually went back and treated a parent for trauma. And that helped resolve their child's disease. And that sounds insane, but it just goes to show again, how the environment impacts you, the childhood, I think was having issues with her asthma flaring.
And the mother mentioned to the doctor that they've never felt really connected to that, to their child. They've never felt the love that they should. And so she ended up going to therapy and figuring out why she was feeling that way. And really dealing with that trauma and learning how to reconnect with her child and having more love in the relationship. So it's amazing what everything can do.
[00:33:58] Leila: Yeah, that is crazy. I now I'm gonna now I'm enticed to go watch the session. So yeah, maybe I'll go watch it as I'm eating dinner later.
[00:34:06] Brittany: There you go. All right, so the next theme is self management. So the term self care, it's trending right now. Everyone wants you to sit on their couch in your sweatpants and eat ice cream and watch TV and practice self care.
But it's way more than that and it's not a fad. You got to make it a routine. So everything you do during your day contributes to your overall health and wellbeing, which means establishing a good routine to manage your stress and living a balanced active lifestyle is crucial. So we all know that establishing a new routine is really hard.
I think it takes like four weeks or something to make it a real habit. But if you've got that routine already established and you've got ways to cope with stress, when you have a difficult day, it'll be so much easier to go find those things and practice them. So, one of the scenarios that really, that they mentioned during one of the sessions that really spoke to me was this idea of space.
One of the researchers coined it, I'll have to put in the notes who it was, but space means sleep, pain, affect, cognition, and energy. And all of those things alone can contribute to a difficult day for an autoimmune patient, but they also impact each other and start a vicious cycle of pain and fatigue. So our ability to understand those symptoms and respond to environmental changes helps you build resiliency and ultimately is what determines how bad or how impactful that disease is going to be for us that day.
So think about it a little bit. This is an example. Your back hurts. You're not going to sleep well because your back hurts, and you don't sleep well, so you're going to be cranky, and you might have brain fog, and then you're tired, and you're in full fatigue because you're just struggling to get through your day, and all you want to do is sleep, but you go to lay down, and your back still hurts, and it's just this vicious cycle, it never stops, and so you've got to find ways, build a routine that helps you combat all of that, and better respond and adapt throughout your day.
So one of the things that they suggested that you practice is positive activity interventions. So that could be like a gratitude journal or spending time outside, making sure you get sunshine, getting up and moving around if you sit all day like me, just really finding those ways to build routine and focus on some of the positive moments in your life can help boost your energy levels, reduce depression and inflammation, and really just set you up for better success.
[00:36:36] Leila: Yeah, that, I mean, we talk about, like, how sometimes having chronic disease is like a full time job in itself. But like, I mean, when you add in all these routines and things like that as well, it's like, even people who don't have autoimmune diseases should try and do these types of things as well, especially with moving around and making sure to not sit for five plus hours and things like that.
It's hard, though. Like you said, establishing a routine is like, I don't know if it's me because I got like, you know, ADHD going on a little bit. But I'm like sticking to a routine is like the hardest thing. But even just being mindful of it, like. Okay, no, I know I need to get up and go do something.
One of the things that I've been doing is trying to schedule like my chores in between my different tasks that I mean, you know, obviously I work from home, so it's easier for me to juggle that. But I will, you know, I'll walk in and work on a task for two hours and then go wash the dishes, or I'll, you know, do a task and then go fold some laundry. And that has really helped to get me up and going and stuff, but still being able to do the stuff that you have to do on a regular basis, which can be very hard to do when you're tired and have pain all the time.
[00:37:48] Brittany: Yeah, well, and everyone wants you to exercise, but it hurts to exercise like we talked about before, but it's going to keep hurting if you don't exercise and when you have that routine you're more likely to be like, okay, I know I need to do these two PT exercises before I go to bed. I can knock those down. But if you're not doing them every day, then you got to remember what they are. And that just adds more stress to the situation. You're like, I'm just not going to do it.
[00:38:12] Leila: Yeah. And I take some time for you to like snap out of it sometimes. Like when I'm in a lot of pain, all I want to do is lay down and then it'll be like a week and a half later. And I'm like, Hey. I probably should have been stretching or doing some kind of yoga or at least trying to move around a little bit. Maybe that'll help. And then I'm like, Oh, I totally forgot about that part.
Like, you're like, I'm doing the rest part. I'm doing good on that. But why am I still hurting? And you're like, Oh, because I really do need to move. So I, sometimes you forget, you really like, there's so many things going on in a given day that it's really hard to keep track of everything, but keeping mind of everything can really help.
[00:38:54] Brittany: Yeah, and remembering to keep it balanced too, because if you've got a good day, all we want to do is go do everything that we've needed to do, and then you end up in a different cycle of, okay, now I'm tired and hurt because I did too much when, because you didn't do anything on the other day, so trying to find a way to balance your activity is also super important and very difficult, especially for people like me.
[00:39:17] Leila: Yeah, no, definitely. Those good days are hard because you know that you're still gonna suffer the next few days after that you're like, I'm just gonna do everything today so that I can get through it. And then you're like, yeah, probably shouldn't have done that. But at least the things are done, right?
[00:39:33] Brittany: Yeah, exactly.
[00:39:36] Leila: But yeah, balance is much better than that. But sometimes that's the best that we're gonna get as well. So we might as well just take advantage of it. So it's hard.
[00:39:46] Brittany: All right, we've got one more theme, and that is to get informed. So, there are multiple sessions that covered the latest research, how do clinical trials work, how does health insurance work, what resources are available, and it's a lot, but getting informed is how you help yourself get the best care and the opportunities that you can.
So, a staggering metric that I heard at the summit was 96 percent of Americans don't understand their health insurance. And who can blame them? It's so complicated. There are multiple plan options. There's multiple ways to get a plan. There's multiple ways to pay for your health care. And there's so many rules on how to get it, how to appeal and they're hard to find and follow.
So something to know is that there are programs in place that no one knows about, like 340B, which is a hot topic here at AiArthritis right now as well, that allows community health centers to get you prescription drugs at a discounted price which is super important to us. The reason that it's a hot topic for us is that those discounts aren't always getting passed on to the patients.
So there's some reform bills to look out for to help make sure that you get those discounts so that you can actually afford your prescription and your care. Something else that they covered was that most hospitals and providers have financial assistance programs, so check their website and see what options that you have or reach out to an organization that can help you find that out, because the last thing we want is for you to need care.
And as we talked about earlier, not be able to pay for it. So, some other areas to get informed about our research and clinical trials. So, if you aren't aware, research and clinical trials are how we've all gotten our treatments. That's how they're developed, how they're tested, and how they ultimately reach us.
But it is, you know, important that you know how research works and what studies to trust and not because there's a lot of publications out there. So something to look out for is that studies are robust, rigorous, and reproducible. You want to make sure that they tested across a lot of people in a lot of different environments, different populations, and that it's reproducible over and over again.
Something else to do is if you can participate in a clinical trial, you could lead to a new treatment being released or an existing treatment being offered to a new disease population. A lot of our autoimmune diseases can be treated by prescriptions or drugs that treat other ones. You know, Crohn's and psoriatic arthritis can be treated by some of the same biologics, but we wouldn't know that if people didn't participate in studies.
[00:42:17] Leila: Yeah, and just to add to that, there's also a piece that we don't talk about as much, but the fact that we need a lot of diversity in these clinical trials because our genes are different. Right. Everybody can react to these drugs very differently. So historically, there have been a lot of middle aged white women that participate in a lot of these clinical trials because that's the main demographic that, you know, RA and these other different, very common diseases have.
But it's also because some of them, you know, have the situation where they can afford to take off work to be able to do these clinical trials and invest that time into their treatment when a lot of other people who may be people of color and lower socioeconomic statuses don't have the luxury or time to even think about being able to take work off to be able to do these types of things.
But it is very important. We found, especially for lupus and other diseases that are more common in people of color, that these drugs don't work the same on someone who's Black versus Asian versus Latino versus white. You can react so differently just depending even on your race. So not only just participating in clinical trials, but specifically, if you want to help represent for your cultural group, that can also be very helpful to make sure that we have a whole picture on what these drugs are doing for these diseases.
So thank you, Brittany, for giving us all of these amazing topics. I did want to go in a little bit more about getting informed and how you can do that with AiArthritis. We have a very popular program that's coming out in less than a month and it's called Go With Us to Scientific Conferences.
Specifically, we will be attending the American College of Rheumatology Convergence in D. C. starting November 14th, so we will be there and we will be on the ground listening to all of these different scientific studies to be able to then translate it to terms that patients can understand and to also let them know how this new research can possibly affect their lives in the next one, five, ten years.
But either way, it is very interesting to learn about the different things that are up and coming in our community. So that is one big way that you can help yourself stay informed on new research. That's coming out is by signing up for, go with us. We have two levels of participation. There is the initial level of participation where we will send you a daily email of all of the different sessions that we attended and our different takeaway points. And then there is the elevated experience, which we always recommend because you get to jump into a Slack group with us, ask us questions in real time. You get to see the behind the scenes and you also get to ask other patients any questions that you may have as well.
So if you'd like to sign up for that program, it is totally free. And you can go to AiArthritis.org/conferences and you will be able to see our sign up for ACR in less than a month. There's also the last episode of this talk show, episode 102 was about the patient journey resources. And it has been our new way to display our resources.
And we've actually created a lot more resources as this is built up. And so if you are looking for information about disease self management, looking for information about exercise, about comorbidities, about how your care partners can get involved in your care. There is a lot of different resources that you can find, and it's divided by the different stages of the patient journey that you may be in.
So undiagnosed or mystery patient, newly diagnosed, currently living with this disease, on the road to remission and care partners. So please take a look at that at aiarthritis.org/patientjourney to get any more resources and information about your diseases or basically how to manage disease.
And you can see more also on our blog about how other patients deal with their disease and their different perspectives that they may have. So that's at aiarthritis.org /blog. Anything else before we go into the final wrap up, any final thoughts about any of the conversations that we had today or anything else that you wanted to say about the Autoimmune Summit?
[00:46:47] Brittany: Even if you don't want to watch the whole thing or read about every session, Go read about When Interest Deal because just one sentence of it can totally change your day. It was amazing.
[00:46:59] Leila: Absolutely. And so as Brittany mentioned in the beginning, by the time this episode is up, we will have all of her blogs that we are cross promoting on her blog and our blog about all of her summaries for the different sessions.
So like she said, if you do not want to go ahead and watch the whole thing yourself, that is totally okay, but making sure to keep yourself informed, like we said checking out our blog and seeing any of the things that may interest you that she has summarized and gotten some takeaway points for us from the autoimmune summit and as well as making sure that you check out any of the other links that will also be in there as well. We have links to all of the different resources that can be helpful. So thank you again, Brittany, for doing the work to be able to provide all of this amazing information to not only the AiArthritis community, but to anybody who is willing to check out our blog and listen to this episode.
I really wanted to say a really big shout out and thank you to Brittany for all of the hard work that you put in on that.
[00:48:01] Brittany: Thank you.
[00:48:02] Leila: Yes. And so, you know, as with all of our work, but specifically this talk show is funded by your donations and all of the resources that we put together are funded by your donations.
So if you like some of the resources that is on our website, or if you enjoyed listening to the rants in this episode, we would really appreciate if you could donate to AiArthritis and help push our mission forward. Because we do not represent the patient voice, we are the patient voice, and we like to make sure that we are giving patients as many valuable resources as we can, so your help and your support will really help with that, and you can go to AiArthritis.org/donate to contribute any amount that you can also sign up for monthly donations where it can be on a recurring basis. You can pay the same thing that you pay for your Netflix account. And that could do the world of a difference for all of the different resources that we could create.
So I would really appreciate if you guys could check out the donation page. And I wanted to let you all know that you can find me at all of our social medias for AiArthritis, but I also do go I do create TikToks and Instagram posts at I go by at lupuslifestyle.lei, so @lupuslifestyle.lei on both Instagram and TikTok.
And Brittany, if you want to let everybody know where they can find you.
[00:49:27] Brittany: Yeah, so you can find me on Facebook, Instagram, or the internet by looking for Chronic Disease Diary.
[00:49:35] Leila: Amazing. And thank you again for joining us today, and we will talk to you soon. Thank you.
[00:49:41] Intro: AiArthritis Voices 360 is produced by the International Foundation for Autoimmune and Autoinflammatory Arthritis. Find us on the web at www. airthritis. org. Also, be sure to subscribe to this podcast and stay up Today on all the latest arthritis news and events.
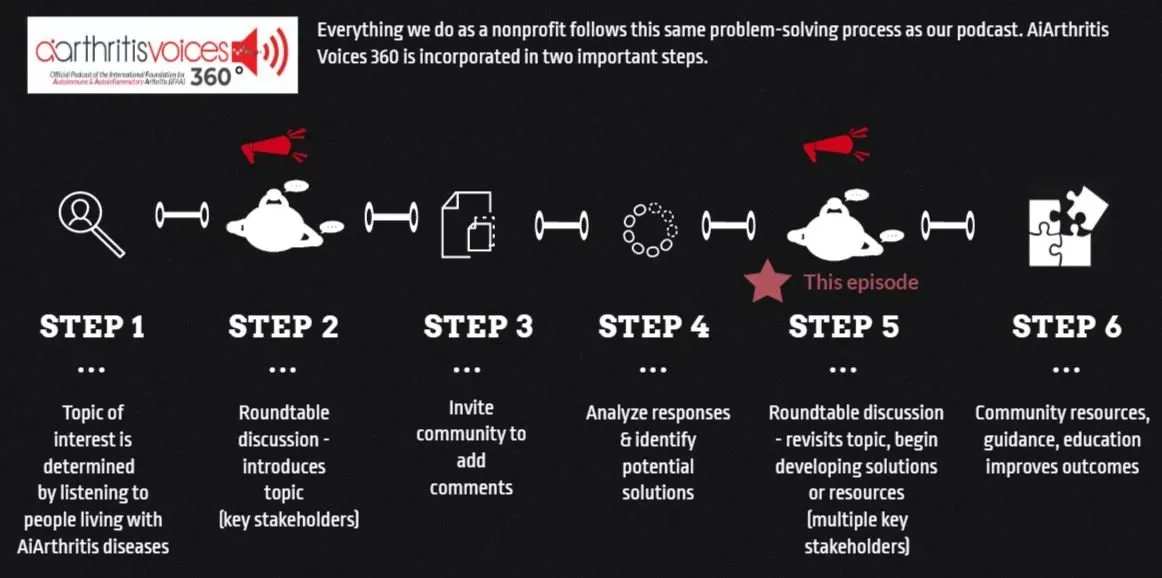
All our main 1st Sunday of the month episodes are either an initial "put the topic on the table" episode (Step 2 in our organization's 6-step problem solving process) or a "revisit to the table" episode (Step 6 in our organization's 6-step process), where we build on a past show because we have moved forward in developing help, tools, or projects around the issue (Step 5 in our organization's 6-step process).
After each show airs we spin off the conversation into many discussions over various formats, which we now call #360its (new in 2022)!
-
Additional Resources & Information
- Submit Your Story or Rant: aiarthritis.org/rant
- Patient Journey Resources: aiarthritis.org/patientjourney
- Advocacy Program Information: aiarthritis.org/advocacy
- Communication Aid for JIA Patients: aiarthritis.org/JIAcommunication
- Follow Our Conference Coverage: aiarthritis.org/conferences
- Read Our Blog for Patient Perspectives: aiarthritis.org/blog
Leila P.L. Valete
Leila is the Health Education Manager at the International Foundation for AiArthritis. She is a person living with Lupus Nephritis and Sjögren’s Syndrome. She is passionate about inclusion and diversity in health education and meeting individuals where they are at in order to learn in a way that resonates with them. Leila is on social media as @LupusLifestyle.Lei sharing bits and pieces about her life with lupus and connecting with others. Connect with her on Instagram or TikTok.
Connect with Leila:
- Instagram: @lupus.lifestyle.lei
- TikTok:
@lupus.lifestyle.lei
Brittany Murray
Brittany is a dedicated AiArthritis volunteer who has been living with Psoriatic disease for over 30 years. She loves to share her story to help others with AiArthritis diseases and to assist with advocacy and education work around hot topics like prior authorization and step therapy. She also started a blog and social community called ChronicDiseaseDiary to build a community of empowerment, love and support for those with chronic diseases or caretakers of those with chronic diseases.
Connect with Brittany:
Pull up your seat at the table
Now it's YOUR TURN to join the conversation!
What do you think about this episode?
We want to know what you think! By continuing the conversation with your opinions and perspectives - we all get a better understanding of the problems facing our community. Better yet, through these conversations we can start working and developing solutions.
We mean it when say 360. Not only do we want your input anytime and anywhere, but we also are eager to see where the conversation will take us. So please, "pull up a seat at the table" and let's start talking!
Email us at podcast@aiarthritis.org, message us on social media (find us by searching for @IFAiArthritis)
Relevant Episodes & Projects
Episode 87: AiArthritis Rant Discussions - Inspired by "Am I the @$$hole?"
Are you tired of feeling frustrated and unheard when it comes to your doctors, your disease, and all the challenges that come with it? Wish you had a platform to let it all out and find understanding?
Submit your Rant!
This is a safe space, free of judgment to get that one thing, or one million things, off your chest and remain anonymous (if you so choose!). We are here to listen to you, your experiences, perspectives, and opinions - we truly want to hear them all.
Ep 101: "Go With Us!" to EULAR 2024
In this episode, our co-hosts bring you an exclusive look into the AiArthritis “Go With Us!” to Conferences program. We dive deep into EULAR 2024, the European Rheumatology Research Conference, where patients and co-hosts reveal groundbreaking advancements in AiArthritis research.
Love the show? Help us make sure we stay on the air by making a donation.
Your contribution helps us continue the work we do every day to improve the lives of millions worldwide.