AiArthritis Diseases and Protecting Against COVID-19 in Healthcare Settings
AiArthritis Voices 360, Episode 99
Air Date: July 7, 2024
This episode is a Step5, as outlined in our 6 Step Patient-Led Problem Solving Process.
In this episode, co-hosts Charis Hill and Jae Walker delve into life after COVID-19, focusing on the unique challenges faced by individuals with AiArthritis diseases. They discuss the importance of continued precautions in healthcare settings, share their own personal experiences, and offer practical advice for staying safe. Tune in for an insightful conversation on navigating a post-COVID world while managing chronic illnesses.
Join us for this episode to gain valuable insights and actionable steps to protect yourself and others in the AiArthritis community.
Episode Highlights:
- Understanding the ongoing complexities of COVID-19 for immunocompromised individuals and those on immune-suppressing medications.
- Jae and Charis share their journey living with chronic disease, their experience with COVID-19 and managing CO-VID prevention now.
- Discussion on recent public health recommendations and the importance of wearing masks, social distancing, and testing.
- Addressing the need for safe healthcare environments and advocating for better protections for high-risk patients.
- Encouraging listeners to resume mask-wearing, improve air quality, and initiate conversations with healthcare providers about safety measures.
AiArthritis Voices 360 is produced by the International Foundation for Autoimmune and Autoinflammatory Arthritis. Visit us on the web at
www.aiarthritis.org/talkshow. Find us on Twitter, Instagram, TikTok, or Facebook (@IFAiArthritis) or email us (podcast@aiarthritis.org). Be sure to check out our top-rated show on
Feedspot!
-
Expand to View the Podcast Transcript
[00:00:00] Intro: Welcome to AiArthritis Voices 360, the podcast solving
today's most pressing issues in the AiArthritis community. We invite you
all to the table where together we face the daily challenges of
autoimmune and auto inflammatory arthritis. Join our fellow patient co
hosts as they lead discussions in the patient community, as well as
consult with stakeholders worldwide to solve the problems that matter
most.
Whether you are a loved one, a professional working in the field, or a
person diagnosed with an AiArthritis disease, this podcast is for you. So
pull up a chair and take a seat at the table.
[00:00:45] Charis: Welcome to AiArthritis Voices 360. This is the official
talk show for the International Foundation for Autoimmune and
Autoinflammatory Arthritis, or AiArthritis.
My name is Charis Hill and I'm one of our podcast hosts and someone
diagnosed with the diseases we represent. My official diagnoses include
axial spondyloarthritis, Ehlers Danlos syndrome, and some other fun
conditions. Today, I am also joined by my friend and colleague, Jae
Walker. Welcome, Jae. Would you like to introduce yourself?
[00:01:24] Jae: Yes, Thank you, Charis for having me. My name is Jae
Walker, and I am also a zebra, like yourself. I'm in a multitude of
wonderful autoimmune diseases. I have rheumatoid arthritis, Sjogren's,
small Fiber Polyneuropathy Hypothyroidism, and it just gets more fun
from there. So I blog I'm an artist, I do artwork around chronic fatigue,
chronic illness, and pain from the patient perspective, of which you are
often a muse for me.
and appear in my artwork as a wonderful subject. And I also love to
speak up and talk about topics that patients love to talk about and are
really important to us that we don't always have a voice about. And that
we don't always have a chance to voice to our healthcare providers and
within the healthcare community.
[00:02:37] Charis: Thank you, Jae. It's so nice to have you here and to
talk to you as a colleague and a friend as well. So I invited Jae on the
show today to have a conversation about the ongoing reality of COVID
19 in our lives, especially for those of us who are navigating healthcare
settings that are no longer requiring masks or doing other mitigation
efforts.
Today we will share some personal experiences. We'll chat about some
of the current public health recommendations for higher risk people. And
we'll discuss some thoughts for how to protect ourselves and each other
from developing COVID 19. Before we begin, I do want to say that
something else to note about our show is that the conversation doesn't
stop here.
We spin off conversations from what is discussed today into what we call
360 its, or breakout conversations that expand on the topic. So watch for
those too as we build out our resources. Jae, I invited you to be a guest
today because this topic is so personal to you. And because you and I
began talking about COVID long before many of those around us did.
I'm wondering if you'd be willing to share what life has been like for you
over the last four years and any other details you'd like to share about
your experience with chronic disease?
[00:03:59] Jae: Well, the first word that comes to mind is struggle. And
the second word that comes to mind is fear. I know that when it all
began back in 2020, I know that you and I started watching what was
happening in China, it was a tremendous amount of fear. I remember
watching it knowing it was going to come here. And seemed to have this
weird concept and weird idea that somehow it was going to defy the
logic of the way viruses work and not show up on the shores of the
United States. The biggest thing, though, for me was I wasn't even
worried about that because I knew it was coming here.
The biggest concern was the way it was working, the way it was
affecting people. And the way it was taking people out immediately with
respiratory infections and the inflammation. We could tell it was
inflammation because we're so familiar with dealing with inflammation
because of our autoimmune diseases.
So it began for me with fear right away and I knew it was It's coming.
And even when rheumatologists, even when my other doctors didn't
seem concerned, I was concerned and I knew that it was coming. And I
remember going to my doctor and talking to them and saying please,
can I get a note asking for me to work from home because of COVID
once COVID hit here in the U. S. and I got a note to work from home and
then a week later lockdown hit in the U. S. and I have actually worked
from home ever since because they actually discovered that my team,
we all work from home, I'm a software developer. We all work on computers. They actually discovered that we work more effectively from
home.
So we're one of the few places that actually saw that and realized it and
stuck with it. Most places opened back up and said, nope, we gotta do
things the way we used to. And you know, everything else be damned.
And so it was scary though. I mean, I just became a hermit. I mean, I
couldn't go anywhere. I couldn't do anything, you know?
And the other thing is that I had a lot of personal trauma and fear
around, around this kind of thing because my mom had actually been in
an accident my senior year of high school and she had been on a
respirator and in a coma for a month. And so it sent me into a tailspin of
anxiety and fear on top of me having a personal understanding of what
inflammation was going to do.
So I had heightened anxiety on top of everything else. So I knew what
this was going to do for me because I had no immune system. I'm taking
medications that wipe out my immune system and I'm seeing people
who have regular immune systems being taken out, putting on ECMO,
you know, going to the hospital and dying.
And then I'm taking medications that are wiping out my immune system
just so that I can barely function, you know, and just so that I can
function on a day to day basis. So I'm, like, wiping down groceries that
are delivered, and I am wearing masks, and I am not in the company of
other people. And it was an extremely lonely and scary time as more
and more people got frustrated and just stopped caring after a while, and
the issue became political, instead of medical, it became harder and
harder for me, because I actually became depressed, because it
became evident to me how many people just didn't care about my life
and didn't care whether I lived or died.
There were people who literally said, well, you know, then disabled
people need to go. They can die, you know, and they didn't care whether
or not people who struggled with health issues lived or died, you know,
and then other people just didn't care because they wanted to be able to
run around and do their own thing and not have to worry about all the
little simple things like washing your hands, wearing a mask out in
public, making sure that you were safe, just doing all of these simple
things.
And these last four years are probably the loneliest, most difficult,
scariest years of my chronic illness journey. And I probably never would
have guessed that. I would have thought that the first couple of years
that I got sick were going to be my worst and my hardest because I had
to adjust. I had to re learn how to be sick and how to move in the world
being a sick person.
I had to re learn how to function and take time out to rest. I had to
relearn how to define my relationships around needing rest and needing
how to function, redefine jobs based on what I could and could not do
physically, redefine how to do everything based on my illness because
there's nothing in my life that my illness didn't touch.
And those first couple of years were the hardest of my life. And I naively
thought those were gonna be the hardest in my chronic illness journey.
[00:10:39] Charis: Yeah.
[00:10:40] Jae: But those were like child's play. These last four years,
ow, chilly, I'm gonna cry. But these last four years have been when I
have felt the most rejected, the most ugly, the most unwanted, the most
lonely, the most scared for my life that I have ever felt.
I have had the hardest diagnoses of my life. I've had to make the hardest
health choices of my life alone and in silos during this time when other
people didn't care whether I was safe or not. And I don't know how to
translate that or make people understand what that's like when they just
want to run around and walk around and act like nothing is wrong and
there's nothing happening and like breathing on me could not kill me.
[00:11:50] Charis: That's a lot. I hear you. I see you. And I want to just
mention to our listeners, you know, at any point, feel free to stop and
drink some water, take a break, and come back to this later, because,
you know we are being very vulnerable here. I'll share briefly that I've
been through similar emotions of, in terms of being isolated over the last
four years, and nothing has changed for me since 2020.
I still get everything either curbside or delivered to my door. I'm fortunate
to have friends who can go into stores for me if I happen to need
something. I haven't been to an in person doctor appointment in years
and I'm really fortunate to have access to telehealth. But anyway, yeah
we're talking about some really deep stuff today and I encourage our listeners to do some self care if you need to do that. So you had COVID
in September of 2023. As far as I know, I have not had COVID, but I
have been sick, really sick during the pandemic with like strep throat and
had to go to the hospital and things like that. But you have had COVID.
Would you like to briefly share more about that?
[00:13:13] Jae: Yes. I had a roommate who did not have the same
vigilance, let's just put it that way, that I did and felt that it was okay to do
things like ride in a lift and pull his mask down and talk to the lift driver
or, you know, go to work and take his mask off at different times if he felt
like he needed to, and he contracted COVID. And he came home and
would always reassure, oh yes, I'm being so safe, I'm being so safe, but,
gave me COVID, and I was so, it was, I managed to not get sick the
entire time until September of 2023 and I felt like I went through every
freaking symptom that there ever was for COVID.
It started with like congestion in my head and I, at one point, lost my
voice. I lost taste. I was fatigued. I could barely walk. I lost my appetite. I
had a migraine so bad. I almost threw up. I couldn't eat for a while. I
reached out to my PCP who is an internal medicine doctor. She actually
regularly reaches out and requests updated notes from my different
doctors, including my neuromuscular neurologist who manages my small
fiber neuropathy.
So she's constantly on top of what's going on with me. And so she was
like, do you have a blood pressure cuff? Do you have an oximeter. You
need to take and take your stats this often. She put a plan together for
me and said, these are your threshold. These are your levels. This is
where we're at. If you hit this level, you need to go into the ER
immediately, we're not waiting because I have asthma, on top of, and it's
not just the asthma, right? That's not just what the, you know, scary thing
is, right? It's but I also do IVIG treatments, which lowers my immune
system even more. Doing my blood work, my immune system is wiped
out. It's like I have the immune system of a cancer patient who has had
their immune system wiped out by, you know, you know, radiation.
That's what my immune system looks like. You know, so she's just, she
was just like, on top of it, on top of it. I hit a point where I was so bad, I
couldn't breathe like, all of a sudden, it hit my lungs. And, I could barely
talk for very long without being out of breath. I couldn't think for very long
without being out of breath.
That was scary. Like you could talk to me and ask me a question and I
could answer you for a few seconds and then I would shortness of
breath would start because I was thinking and I was like, I had never
experienced that before. She said, we have to get you on Pax Lovid.
Like we have to get you on this, like right away.
And of course my insurance required a prior authorization for Pax Lovid.
[00:17:12] Charis: I love it. I love this. It's great.
[00:17:14] Jae: Yeah. So with everything that I'm taking and everything
that I'm on and all of the unusual and rare medications that I'm taking, I
still required a prior authorization. Oh, I hate my insurance. And I got
approved and got the medication just in time. I was about, she was
about to send me to the hospital because my breathing and everything
was so bad. I took the Paxlovid and she was like, Okay, if your numbers
don't improve by tomorrow you're going into the ER tomorrow. Because I
had developed bronchitis within three days.
I had bronchitis, which is apparently what happens to me now when I get
sick. I develop bronchitis now every time. It's been my, my pattern now
for a couple of for years now. And so once I got the Paxlovid, Then the
symptoms started to get better, but the breathing did not get better, and
the shortness of breath did not get better.
It was like it kind of evened out a bit. The downward spiral stopped. It
just kind of, it's kind of, it was kind of like I was being thrown down the
stairs, and I suddenly stopped in the middle of the stairs, and I stayed
there. That's kind of what it felt like. And then I had to pick myself up and
start trying to climb back up the stairs, but I was still on the stairs, you
know, so I couldn't breathe and I was so fatigued.
I couldn't walk across the room and I created several pieces of artwork
around this and did a blog for Creaky Joints around this about what it
was like, what it felt like to try to breathe with this with COVID. It was
unbelievable. It was like nothing I've ever felt before. I actually went to a
long COVID clinic recently and have been diagnosed with long COVID.
And I now actually have mass cell activation syndrome because of it. So,
my immune system is all whiffed up into a frenzy and I have to carry an
EpiPen with me and my inhaler with me at all times because my body
freaks out at all different kinds of things and I can have a life or death immune reaction to things because my body The inflammation levels
are, like, whipped up to a frenzy now, all because of COVID.
[00:20:05] Charis: That's a lot. Thank you for being vulnerable with all of
that. It's a lot of information to share about your personal journey, and
I'm sure our listeners are appreciative of knowing more, while also
potentially being horrified that this all happened to you. So thank you. I
mean, I can only relate in terms of being isolated and afraid of getting
what you had.
So, I am also on immunosuppressive medications and even before I
knew I had axial spondyloarthritis. As a kid, I got really bad pneumonia
in middle school I wasn't on immunosuppressive meds at the time
because we didn't know I had a chronic disease, but we do know I have
an autoimmune disease now, so that was probably what happened, and
I was delirious, I should have been hospitalized, I can't speak today and
I was in bed for I think three weeks, and so I know.
That if I get a respiratory illness, it will get bad really quickly. And so I've,
and I've been fortunate, like I want to recognize my privilege at being
able to stay home, I don't have to go to work in person, I don't, I'm not
forced to go to grocery stores because I do have access to curbside
delivery.
Hearing stories like yours, and knowing that your story is not
remarkable, because it has happened to so many people, makes me
concerned that so many things are going so called back to normal,
where there are no mitigations in place. And so, I want to transition into,
The next part of what we're going to talk about, which is like, basically,
why are we talking about COVID on this show?
What makes it unique to our community? I think we've already
addressed that. The fact that we are both immunosuppressed because
of medications we take, we fall under that high risk umbrella. Many of
our listeners are also on medications that suppress their immune
system, or they are immunocompromised without having to take
medications.
And in other ways, people are considered high risk. So I want to bring up
a quote from one of the blog posts that you wrote on Creaky Joints in
this February, actually. And you kind of touched on this when we started this episode by talking about, like you and I starting to talk about COVID
early on, but so here's the quote.
Quote, I began studying patterns of the virus when it was wreaking
havoc in China and had not decimated the U. S. yet. I read everything I
could get my hands on. When it came to the U. S., I had the Johns
Hopkins virus case counter up on a tab in Chrome at work and home. I
could and did educate various doctors that I saw for treatment, unquote.
Are you still educating doctors, Jae?
[00:23:25] Jae: I'm still educating doctors why I have to wear a mask.
Like, for example, I'm having issues with my small fiber neuropathy and
I'm having my spine is compressing. Spinal stenosis and some other
things going on. And I just had some SI injections done. And I requested
that my pain management doctor and his small little team of nurses, like
two nurses in the room, that they all wear masks.
I wear a mask. I can't have anesthetic because no one I swear a lot
normally and I'm doing, I feel proud of myself because I'm trying to keep
that under control, but it makes me very angry. So I'm trying not to
swear, but like they, they don't wear masks. Okay, so for, and I can't go
under for anesthesia.
Now, I really need anesthesia, even though it's a local, but I need
anesthesia for something like this because of my fibro. When they do a
local for an SI injection for me, fibro kicks back and makes me flare and
makes it worse. So in reality, I really need to go under so they can give
me an injection and I can get the full effects of a nerve block.
But now, because no one is wearing masks, I can't do that. So I have to
wear a mask and be fully awake and not get the full effects of an SI
injection. And I had to ask my team if they can wear masks. So there are
two procedures I've had. One was a trigger point injection that they did
first a couple of months ago and oh, they were willing.
Okay, fine. Yeah, we could put a mask on for you oh, no big deal. Oh,
and they were happy to do it blah blah blah And then this last time when
I asked them again to put a mask on well, my doctor was freaking
annoyed that I asked for it. Is there a reason you need a mask? Why do
we need that? You do you have an immune system?
Is there a problem? So I'm sitting there, vulnerable, in pain, laying on
my stomach, waiting for this injection, trying to explain to him because I
see a nurse practitioner in his office and he's the one who does the
injections. He's the one I see regularly. And I explained to him, okay, if
you look at my blood work, I have no immune system.
I need for three people to not stand over me and breathe on top of me
their germs because they are in close proximity to people all day long.
And you could be carriers of COVID, of the flu, of RSV like of anything
else, strep. Strep is so bad. We could die from strep, just from the
immune medications that we take.
Not even just COVID. But, you know, read the inserts of your
medication. Read the inserts. It's right there. Chicken pox, people can
die from chicken pox. Even if you've had it. It's right there. And so I have
to educate my doctor. Yes, I need you to wear a mask because I can't
have you breathing on me. And he was not happy and he sloppily put his
mask on.
And he did the injection. And I was so mad.
[00:27:39] Charis: Yeah, unfortunately, I've had similar experiences and
I don't want to go through all of the stories because there's so many,
because I want to, you know, our listeners are probably fully aware of
that because I have so many stories that I'd love to share, but I can't.
We could do a whole show just sharing stories, I know. And it's difficult
to navigate those situations as people who are educated and also
receiving care and wanting to be respected and receive care and also
safe in terms of protection for viruses, but also safe from harassment.
And sometimes we have to navigate like okay, what's the better option
right now? Is it to advocate for safety with the mask, or is it to advocate
for care and forego the fight for the mask? Because and we have, we do
have a lot of healthcare professionals who listen to this show. And so I'm
wanting them to be aware that we do juggle, you know, what's more,
what is the priority, just like they juggle, what's the priority?
Do we treat the patient with this or that? Anyway I want to shift a little bit
to talking about current public health guidance. But before that, I want to
share three facts that I found interesting recently regarding COVID. So,
number one, as of May 1st, hospitals are now no longer required to
report COVID hospitalizations to the CDC.
So we now don't really know how many people are being treated in
hospitals for COVID 19. The second, is that across the country,
wastewater data are showing COVID levels rising. And I'm in California
and San Francisco recently reported some of the highest concentrations
of COVID in wastewater that they've ever measured so it was in early
June. And the third thing is something that is in the news a lot lately,
which is that there are states that are now considering making wearing
masks illegal. So North Carolina and New York are top of mind. I'm from
North Carolina, so I'm paying attention to that one a lot. And who knows
what the outcome of that will be by the time you are listening to this.
So having said this yeah, New York. So Mayor Eric Adams has talked
about trying to ban masks in New York for months now. And I think was
working with businesses to try to ban them and I think now it's sort of
moving up towards the legislature. Yeah. So having shared all that but
where, what is the current public health guidance?
Like what is the current context? So I want to start with the CDC. On the
CDC webpage that gives COVID guidance for people who are
considered high risk, the first directive says, quote, if you have one of
these conditions, talk with your healthcare provider about how best to
protect yourself from severe illness from COVID 19, unquote.
Jae, we're on that list. People who have suppressed immune systems
are on that list. We can talk about this, can't we? I mean, so it's kind of
obvious that based on that first directive, talk to your healthcare provider.
If you're on that list, it's important for rheumatologists, for dermatologists,
for other specialists who treat people with AiArthritis conditions to be
knowledgeable about what many of us who are immunosuppressed or
immunocompromised experience and what we need. So anyway, I know
that you're wanting to share some thoughts on that so go ahead.
[00:31:58] Jae: Well, I mean, I think it's important, especially if we do
have healthcare providers who are listening to this. I think one of the
things that I would want to stress is that they need to make it a safe
space for patients to talk about this kind of stuff, a very safe space,
because that's the biggest thing is patients very often don't feel safe
discussing things.
They feel afraid to talk about things, especially something like this. One
of the things is that you know, maybe, first and foremost, a healthcare
provider might have to be the one to broach the subject to bring it up and discuss, you know, Are you taking necessary steps? Are you feeling
safe? Are you able to mask when you need to mask?
You know, that would be a huge weight off of a patient's shoulders
because we're already juggling so, so much. We're tired. We're fatigued.
Chronic illness patients, especially. We juggle and we wake up in the
morning and we have to figure out what we have the energy for. We
have to figure out what we have the strength for, and if we have to go to
a doctor and feel like, okay, maybe we have to educate them or talk to
them about something that's difficult, it isn't just that day.
We actually spend time and energy ahead of time preparing to talk to
that doctor. So it's time and energy ahead of time. And with these
directives, these are confusing. Because you have the CDC telling us,
okay, we need to talk to our doctors, yet the spaces that are supposed to
be safe for us are pulling out and not supporting us in ways that we need
support.
Like, now hospitals are not going to be doing it, and, you know, states
now are considering banning masks. It's I mean, what are we supposed
to do with that? How are we supposed to deal with that? Me, I have to
wear a mask every time I go out.
[00:34:42] Charis: Yeah, me too.
[00:34:43] Jae: I've created artwork around that. I have a piece of
artwork called Bullseye because I feel like I have a bullseye on me when
I go out, no matter where I go.
I go with doctors who deal with high risk patients, my allergist, my
rheumatologist, you know, endocrinologist. Doctors who deal with
patients who are in a situation where they should be wearing masks.
Now, there are patients there who wear masks, but the doctors aren't
wearing masks, and the healthcare providers, where I see my doctors,
none of them are wearing masks.
[00:35:34] Charis: Yeah, and it's getting It's confusing, and it's difficult,
and it's scary. Yeah, those are really good for us. Yeah, for sure. Yeah,
bringing up the whole fear part and being tired extremely valid and I
think a lot of our listeners can relate to you know, it takes energy to plan
for how to self advocate it takes energy to recover from self advocating it
takes us. I Didn't realize until my first outing.
And this was in 2020 when people were supposed to be staying home,
you know, and I remember just going with my partner at the time just for
like a drive and realizing how much energy it took just to leave the house
now. Like it takes energy to leave with a chronic disease sans COVID
being the reality.
But with the public generally being an unsafe space for us, it's like
exhausting because you're mentally preparing and then you're mentally
experiencing and then you have to recover. But I'm going off topic a bit
on a tangent, but it's so valid to remind health care professionals that we
are juggling what the priority is when we're in that appointment that
hasn't changed and with the reality of COVID mitigations going away,
that's just adding one more thing to the list that we juggle. I want to bring
us back a bit to another part of the CDC website, which is the CDC page
on how to protect yourself and others. This was updated April 4th, 2024.
And the recommendation is that you wear a mask, distance, and test
when around high risk people.
Okay, so the thing is, how do you know when you're around high risk
people? That's right. Actually, like, I think the easier question might be
how do you know when you're not? Like, for example, like the CDC list
includes people like us who are immunocompromised, people who are
disabled, But it also includes conditions and situations like depression,
pregnancy, and smoking.
Yeah I mean, like, it's just funny to me how people just assume that
disabled people don't exist in public. Yeah. Like, oh, I'm fine not wearing
a mask in the grocery store. There are no high risk people here. How do
you know that? Yes. So I always joke about how the CDC is telling on
itself. Like it's really saying you should be doing these things all of the
time because high risk people are everywhere, except that's not how,
that's not what they actually mean.
Anyway, I just could not bring that into this conversation.
[00:38:46] Jae: Because if we're really following their recommendations,
like, that's what we would be doing. Everyone would still be masking,
and we would, in public, in, in any place where there's, like, that's just
what we would be doing. Right. You know I don't go on Facebook much,
but I was on Facebook, and there was a friend in Asia, and I mentioned
how I'm frustrated because I now actually have an in homes barometer
to test my asthma because since all of the guidelines and requirements for masks and stuff went away, I can't test my breathing at my allergist /
immunologist's office because not only do they not require masks, but
somebody will come in coughing and hacking and they won't get up.
They have masks right there that they offer people, but they won't get up
and go over and require that person to put a mask on. They'll just let
them sit in the waiting room hacking and coughing and spreading
whatever it is that they're spreading.
And, I'm like, I can't take my mask off. Take a deep breath in, and
breathe into this machine you want me to breathe in to test my breathing
because I'm gonna suck all this air in. And, not only do I not, I mean you,
I can't believe that you run an office like this and I, I mentioned
something about how they don't require masks in that office and this
friend of mine who lives over in Asia was horrified and said, I absolutely
can't believe that.
They know everyone here wears masks and no one has stopped
masking, and they still wear masks over here in Asia out in public. They
wear them in doctor's offices, and they wear them out in public. No one
goes without a mask. And it's just, they were just horrified. And I'm like, I
don't, I'm horrified too, because I, so now I have to spend a co pay every
month now, so that I can have an in home handheld device so that we
can know how bad my breathing is because I can't do it in the office.
[00:41:24] Charis: Yeah, I, that actually brings to mind the financial
implications of what like, we are financially impacted by healthcare
environments being inaccessible, whether it's to pay for extra healthcare
costs like co pays, or if we're delaying or foregoing care and it ends up,
like, affecting us down the road where it'll be more expensive on us.
And on the health care system and I feel like we could do a whole
episode on that and maybe that can be a spin off one of the 360 it's I
mentioned earlier cause we just don't have time to go into it today, but
that is a really good point to, to put in there. Considering all the impacts
on patients who are high risk it's mental, it's physical, it's emotional, it's
financial.
And that's just the healthcare related side and we could do a whole other
spin off on just the social side of just existing you know, in public and in
our day to day lives so that we don't run out of time. I do want to shift to
some, like, you know, how can we be proactive a bit and like, so
considering what we've talked about, all the personal stories we've shared, the systemic issues we've shared some of the public health
guidance we've shared.
What do we do about the current state of COVID and accessing
healthcare as high risk people? So let's do like three, three things that
we can do individually or systemically. I know I'm putting you on the spot
here.
I can start if you don't want to, if you want to think about it.
[00:43:24] Jae: Yeah, you start and go ahead. Give me a minute.
[00:43:27] Charis: Sure. Welcome to Charis hosting Podcasts. They put
you on the spot. So, well, so in my notes for this show I wanted to bring
up the Americans with Disabilities Act and the fact that the ADA does
guarantee equality for all in health care, you know, access, basically
disabled people have the right to access health care and have
accommodations to access health care equitably and safely. And that
includes respiratory viruses. So I actually looked up the people's CDC
website and they have a letter template where people can write an
accommodations request for a doctor's appointment.
There's a template and you can fill out, you know, what makes sense for
you. On it are things like air purifiers, testing before the appointment,
and these are for the health care environment and health care providers,
N95s, being able to enter a side door. I can't remember what else, but so
there are resources out there to request ahead of time accommodations
and that way it's on paper.
It can go in your file as a request that you can refer to later. You can
request a response in writing. I actually have a story about requesting
accommodations and it did not go well. And I do hear stories where
things like this don't go well, but it doesn't hurt to try and the more of us
who do it, the more likely I think.
So, I think the second thing is actually from the CDC High Risk
Guidance page, their last sentence is quote check with your healthcare
provider about safety precautions for office visits and ask about
telemedicine or virtual healthcare appointment options, unquote. So,
that's another thing you can do.
And I'll say my third one is sort of more, it's personal with an individual
as well as systemic. And that's like just sort of a list, like, okay, wear
masks. It's okay to just restart wearing masks. If you stopped, you can
just restart. It's easy. Test do air filtration for the doctors out there I and
Jae mentioned this earlier, actually, I wrote this in the notes. I have a
personal plea for you to initiate conversations with patients about
COVID, about long COVID, about their immunosuppression and high
risk and please wear N95s. Don't make a patient ask for them. And then
like I said, on a systemic level, advocate for mitigations to either
continue or come back.
The People's CDC has some resources for that. The World Health
Network has some resources for that. And maybe, like, work on an
airborne infection mitigation protocol for your own organization or
business or group. You can go above and beyond what the current
public, official public health recommendations are.
Did that bring up anything to mind, Jae, that you wanted to share?
[00:46:57] Jae: Yeah, I think there are a couple of things. Sometimes it's
hard for people to advocate for themselves. So I think it's good to think
about stuff ahead of time, figure out what is important to you. Well,
here's one thing that I do. So I have masks at home and I keep them
handy by my front door.
So I live in an apartment, right? And when I have, no one comes in my
front door without a mask, period. So what I do is like, if I put in a
request that something has to be cleaned or fixed or whatever, they
come to my door. I greet them at my, like I put in a request and I say
they have to wear a mask. If they come to the door and I say, Hey, do
you have a mask?
If not here, I have one for you. So I will provide a mask. So one of the
things that you could do is show up to your doctor's appointment with an
extra mask, right? You could have one in your pocket. There's no harm.
I've asked doctors before, can you wear a mask? And they have put
them on for me for the appointment.
Right? And I've asked them several times and then after that they just
remember and they'll do it for me. So I have doctors who do that and
sometimes, you know, I know there are people who are a little bit more introverted. So maybe sometimes, maybe bring somebody with you who
can sort of help you, give you courage and right?
Who can kind of be your backbone or just be in the room with you if you
need them to while you ask for the things that you need to ask for, right?
You can kind of bounce ideas off of them and say and just have a short
conversation with your doctor. Say, Hey, I am just like what you were
saying, Charis, I really need to feel safe.
And in order to feel safe, I really need you to wear a mask with me, but
bring somebody with you. So that, and then you also have a witness to
whether or not that doctor says yes or no. So that's also good to have in
your corner as well, right? Because there are some amazing doctors out
there, but there are also some doctors who sometimes they will bend if
they have an audience, whereas they would not bend otherwise.
Let's just put it that way.
[00:49:35] Charis: I want to mention that all of our listeners who are
doctors are amazing. I'm 100 percent positive. That's right. We right.
Yeah,
[00:49:48] Jae: but sometimes, you know it's, it can be hard to advocate
for yourself. I would say write down your points in a notebook, bring a
notebook with you with the points that you want to ask for.
I think that's really good. You can. You could have a sheet of paper and
say, hey, can you put this in my file? Because this is important and this
is like what I need. So that they know from here going forward, like you
need masks, right? Anybody who deals with you, they need to wear a
mask. It's not just the doctor, it's the nurse too, right?
Just whoever it is. I don't know I'm focused on kind of on the patients, I
guess because I know that it's not always easy to speak up for yourself,
and it's not always easy to kind of get there. So maybe you could also, to
help you, and to support what you're saying like what Charis you have
pointed out, is maybe print out what the CDC says.
Right? For what immunocompromised patients should do. Print that out
as proof. And then take that to your doctor and say, Hey, this is what I
feel comfortable doing, and here's proof. Right? Because sometimes
that's what doctors need. They need proof. I have a doctor who is like that. I can ask and plead and do whatever, but if I show him data and
information, then he will, we will go there and that's what will happen
with my doctor.
So that's a good one, too. So you can print out data and information like
the CDC website and information like that. So I think that's a really good
one too, is to bring them proof that this is what immunocompromised
patients should be doing. This is what should be happening for our care.
So I think that's a good one too, to sort of have in your back pocket and
show and say, look, this is the kind of care that I deserve and that I
need.
[00:51:56] Charis: Yeah. Those are some really good suggestions.
Unfortunately, I believe we are out of time. We have filled this episode
with so much and there's so much to continue this conversation about.
To our listeners, please let us know if you'd like to hear more on this
topic and tell us what stories of your own do you have?
What's worked or hasn't worked for you? We always love hearing from
our listeners. And I think that's a wrap. Jae, thank you so much for
joining me today at the table. Thank you so much for having me. I
always love talking to you.
[00:52:34] Jae: And we could talk about this topic forever,
[00:52:37] Charis: obviously. Totally. So where can people find you?
[00:52:43] Jae: These days I am. You can find me on Facebook under
Unexpected Advocate. I am also on Instagram under Unexpected
Advocate. And then you could find me on Threads under J A E L E A H.
Walker. W A L K E R. And my artwork is spread out all through there
along with my blogs and all my stuff's just there so you can see some of
my stuff.
And on CreakyJoints org they have my artwork and stuff.
[00:53:20] Charis: Awesome and I do encourage listeners to check out
their artwork. It's amazing and I'm kind of partial because I'm their muse.
So awesome. So listeners make sure to follow our posts on social media
about this topic and comment or message your own experiences or tips.
We can be found on all platforms, Facebook, X, Tik Tok, Instagram,
LinkedIn at I F A I arthritis. That's @IFAiArthritis, you can check out this
episode in all episodes along with our amazing patient design programs
and resources at aiarthritis.org. And while there, please click that big red
donate button because we couldn't do the work we do without your
generous support.
Thank you all again for tuning in and we hope you learn something new.
[00:54:18] Intro: AiArthritis Voices 360 is produced by the International
Foundation for Autoimmune and Autoinflammatory Arthritis. Find us on
the web at www.AiArthritis.org. Also, be sure to subscribe to this podcast
and stay up to date on all the latest AiArthritis news and events.
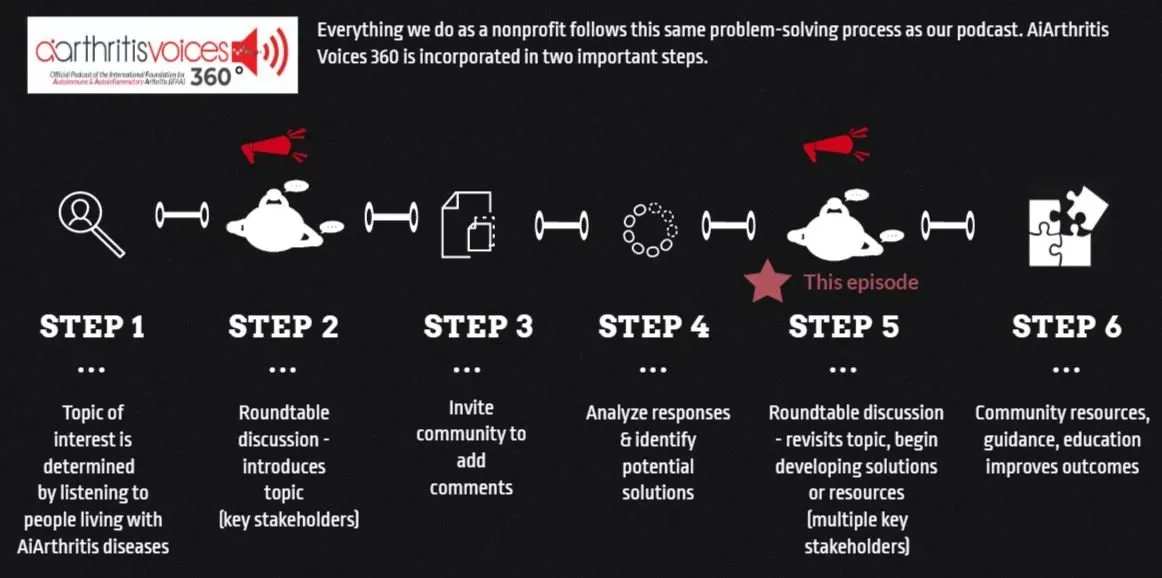
All our main 1st Sunday of the month episodes are either an initial "put the topic on the table" episode (Step 2 in our organization's 6-step problem solving process) or a "revisit to the table" episode (Step 6 in our organization's 6-step process), where we build on a past show because we have moved forward in developing help, tools, or projects around the issue (Step 5 in our organization's 6-step process).
After each show airs we spin off the conversation into many discussions over various formats, which we now call #360its (new in 2022)!
-
Additional Resources & Information
- Volunteer with AiArthritis : https://bit.ly/AiArthritisVolunteerApp
- Donate to Support the Show: https://www.aiarthritis.org/donate
- Sign up for our Monthly AiArthritis Voices 360 Talk Show newsletter! HERE
- Follow AiArthritis on all social media platforms @IFAiArthritis
- Jae’s blog - When I Had Co-Vid: https://creakyjoints.org/living-with-arthritis/coronavirus/patient-perspectives/when-i-had-covid/
- COVID Keeps Rising in Bay Area Wastewater. What to Know, From New Variants to Symptoms: https://www.kqed.org/news/11987343/covid-bay-area-wastewater-variant-symptoms-isolation-guidance
- CDC “People with certain medical conditions” page: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html
- CDC page “How to protect yourself and others” https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html
- People’s CDC resource page for requesting COVID healthcare reasonable accommodations: https://peoplescdc.org/2023/05/09/ada-rights-workshop/

And now, let's 360it!
The main Sunday episode is where we "put the topic on the table," but it's not where the conversation ends! Now we spin off the conversation into different discussion segments. Below you will find several 360its. Some are videos from the main episode, while others are audiograms (soundbites).
Soon we will be launching additional 360its, which will build on these conversations. We'll hear from patients in the United States, Canada, and Australia who are here to help you through the transition to biosimilars. We are also planning a WATCH PARTY, where we will play back segments of webinars that aim to teach you more about biosimilars - and you'll have your fellow patients at AiArthritis to talk through it all with you! Stay tuned.
360its & SHORT VIDEO CLIPS FROM THE MAIN EPISODE (Coming Soon!)
Charis Hill
Charis Hill, who uses they/them pronouns, is a disability activist, writer, speaker, and model living with conditions such as Axial Spondyloarthritis and Ehlers Danlos Syndrome. They use narrative engagement to advance social justice for multiply-marginalized disabled people and have been featured internationally in media and the documentary "Becoming Incurable." Charis has written for HealthCentral, Healthline, and Business Insider, and has been recognized by the Arthritis Foundation and Spondylitis Association of America for their advocacy work.
Connect with Charis:
- Twitter: @beingcharisblog
- Tikok : @beingcharisblog
- Facebook: @beingcharis
Jae Walker
Jae Walker, who uses they/them pronouns, is a blogger, writer and artist living with conditions such as rheumatoid arthritis, Sjogren's, and small Fiber Polyneuropathy Hypothyroidism. They are an advocate and artist sharing artwork around chronic fatigue, chronic illness, and pain from the patient perspective.
Connect with Jae:
- Threads: @JaelehWalker
- Instagram : @UnexpectedAdvocate
- Facebook: @UnexpectedAdvocate
Pull up your seat at the table
Now it's YOUR TURN to join the conversation!
What do you think about this episode?
We want to know what you think! By continuing the conversation with your opinions and perspectives - we all get a better understanding of the problems facing our community. Better yet, through these conversations we can start working and developing solutions.
We mean it when say 360. Not only do we want your input anytime and anywhere, but we also are eager to see where the conversation will take us. So please, "pull up a seat at the table" and let's start talking!
Email us at podcast@aiarthritis.org, message us on social media (find us by searching for @IFAiArthritis)
Relevant Episodes & Projects
Episode 60: COVID Blues: It's ok to ask for help
This week, join your patient co-hosts Kelly Conway and Rick Phillips and special guest Heather Kenjorski, a licensed social worker, for a frank discussion about mental health, AiArthritis patients, and the COVID-19 pandemic.
Episode 29: COVID-19 and AiArthritis
In this episode, Tiffany and Danielle discuss the current spread of the virus and Danielle explains the concept of epidemiological models and flattening the curve. They discuss the efforts to reopen some areas that had been previously locked down, as well as how you can protect yourself from infection if you live in one of those newly opened places.
COVID-19 Vaccinations, Shared-Decision Making, & Rheumy Communications
This week join your patient co-hosts Tiffany and Deb, as they welcome Al and Jeff (Dr. Al Kim and Dr. Jeff Sparks) to talk about the latest in COVID-19 research and vaccinations, including variants, antibodies, and the importance of communicating with your doctor about boosters and the evolving landscape (shared-decision making).
RheumyRounds SPECIAL EPISODE - COVID-19 & Vaccisnations Communication, Education & Shared-Decision Making
Patient Co-Hosts Tiffany Westrich-Robertson & Kelly Conway are joined by Dr's Al Kim, Vibeke Strand, and Jeff Sparks as they discuss patient and rheumatologist vaccination hesitation and key education points, while providing insights to assess benefits and risks and promote shared-decision making strategies.
Love the show? Help us make sure we stay on the air by making a donation.
Your contribution helps us continue the work we do every day to improve the lives of millions worldwide.