[00:00:00] Tiffany: Welcome to AiArthritis Voices 360, the podcast solving today's most pressing issues in the AiArthritis community. This is a special rebroadcast of our inaugural RheumyRounds episode, where we discuss the communication barriers that currently exist between patients and their rheumatologists. Head to Arthritis.org/RheumyRounds for more great episodes from this series and opportunities to
join the conversation, that's AiArthritis.org/RheumyRounds. Pull up a
chair and take a seat at the table. We're so happy to have you joining us at the table today. We have a special episode. We're doing a a pilot episode here, testing out a new series we hope to launch and keep it going strong called RheumyRounds.
My name is Tiffany. I am co hosting today with Kelly. Kelly, why don't
you say hello? Hello, everybody. And, Kelly and I are both co founders
at the International Foundation for Autoimmune and Autoinflammatory
Arthritis. So we are also people living with these diseases. I myself am
diagnosed now, which time with non radiographic axial spondyloarthritis,
prior seronegative rheumatoid arthritis, lupus has been thrown in there
before, Sjogren's, all kinds of things but Kelly, you also have diagnoses.
Sort of.
[00:01:30] Kelly: I, yeah I think right now they have it listed as
rheumatoid arthritis, but I've had psoriatic arthritis, lupus has, I was
called lupus light for a while. I don't know what that meant, but it's like
diet Coke, I guess. And then so now we're, I'm sticking with rheumatoid
arthritis, fibromyalgia, Graves disease. Just a hot mess over here.
[00:01:54] Tiffany: Oh, okay.
[00:01:55] Kelly: There you go.
[00:01:56] Tiffany: All right. Well, before I talk a little bit more about what
these RheumyRounds are, let's meet our guests today. We have a
couple people joining us. One is Dr. Alfred Kim, who is my
rheumatologist. Hey, Dr. Kim.
[00:02:12] Dr Kim: Hey, how you doing?
[00:02:14] Tiffany: And then we also have Jerik, and I, gosh, darn it,
Jerik, I don't, oh, how do you say your last name?
I didn't ask before we started. Oh, it's all right. It's Leung, Leung. All
right. And we have Jerik Leung and Kelly's going to tell you a little bit
more about their backgrounds.
[00:02:29] Kelly: Okay. Well, Dr. Alfred Kim is an assistant professor of
medicine and of pathology and immunology at Washington university
school of medicine.
He also founded and directs the Washington university lupus clinic. Dr.
Kim's research group is focused on addressing the unmet needs of the
human systemic lupus erythematosus SLE, including understanding and
leveraging of the biomarker potential. Okay. of complement activation
products, testing novel noninvasive imaging platforms such as photo
acoustics to detect lupus nephritis, understanding the relationship
between sleep quality and lupus activity and restoring eroded social
support in patients with SLE.
Welcome to Dr. Kim.
[00:03:10] Dr Kim: Thank you.
[00:03:11] Tiffany: Welcome.
[00:03:12] Kelly: Next we have Jerik Leung. Jerik is a graduate student
in the Master of Public Health program at St. Louis University, College
for Public Health and Social Justice, focusing in behavioral science and
health education. He's been involved with lupus related health research
for the past four years, beginning during his time as an undergraduate
student at Washington University, where he met Dr. Kim and conducted
a senior thesis project in medical anthropology, seeking to understand
the primary obstacles of living with lupus. From the patient perspective,
this work and the necessity of the patient voice in guiding research and
treatment priorities has formed the basis of Jerik's current work with Dr.
Kim and Dr. Elizabeth Baker, who is a professor of behavioral science
and health education also at St. Louis University. They're working on
understanding and developing interventions related to social support and
impact on quality of life among those living with lupus using a community
based approach.
After graduate school, Jerik intends to continue on in a career path in
health sciences research with a specific focus in autoimmune diseases.
So welcome to Jerik as well.
[00:04:15] Jerik: Thank you.
[00:04:16] Tiffany: Welcome and yay to the specific focus on
autoimmune diseases. I have to do a shout out to that. So I'm going to
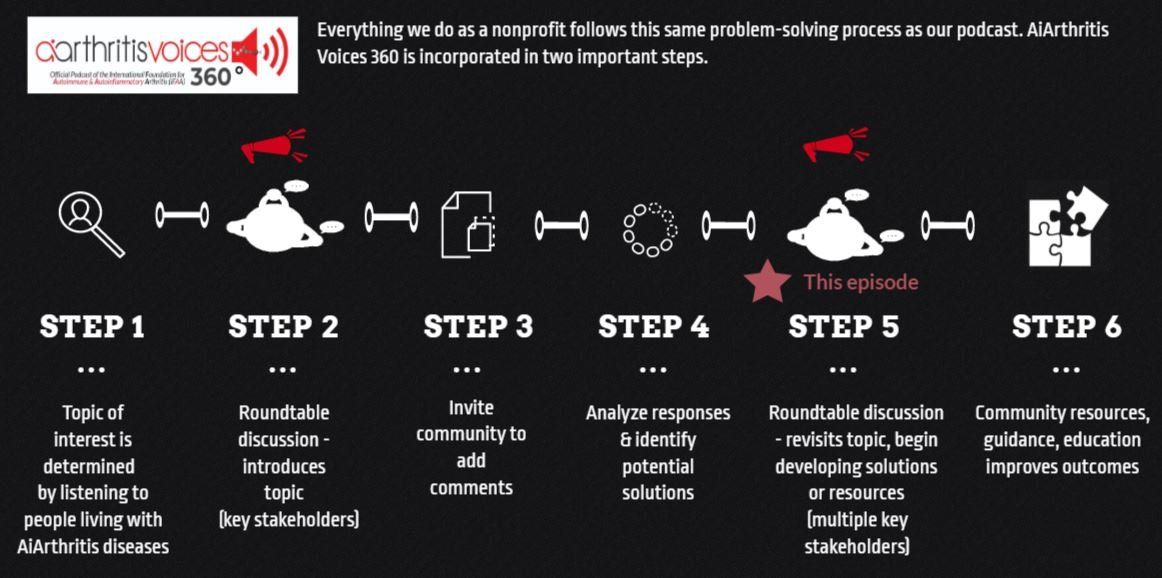
circle back really quick and, and tell everybody a little bit about the vision
here of, of RheumyRounds and, and how it came to fruition.
We have patients that we asked to submit topics for podcasts and a lot
of patients submitted the need for communication improvement between
the patient and the rheumatologist. There were a lot of different
subcategories that came up. And it was that moment that we said, wow,
there's so much that needs to be improved.
Maybe we could do a whole series called RheumyRounds. And the
whole concept of roomie is first of all, because patients call their
rheumatologist Rheumies , but it also. is a word that envelops the entire
rheumatology community. And that could include researchers, that could
include other doctors that work with the researchers.
So we're trying to keep the scope broad so that we can include all of the
relevant topics. This series would be aimed at improving
communications between patients and rheumatologists and people in
the rheumatology community. And the concept really mimics the way
that we work at our nonprofit, it, which includes patients who use our
professional backgrounds to facilitate conversations between various
stakeholders and a global pool of patients.
And those are people like us living with autoimmune or auto
inflammatory diseases that include arthritis as a major clinical
component. We also like to host these kinds of conversations because
different viewpoints are vital to problem solving. And we like to say at
IFAA that we are problem solvers.
So in order to do that efficiently, you have to have all parties at the table
and listen to those different viewpoints and invite other people after
these conversations to then submit comments so that all voices and
perspectives are considered. And then essentially we develop solutions
and resources that matter most to everyone, see how that works. Isn't
that fantastic? So that is how RheumyRounds was envisioned. And we
welcome you to the first episode. Today's topic is improving patient
Rheumy communication with typically patients talk to each other about
what's important to us and choosing or keeping in some cases, the right rheumatologist, which often revolves around how our expectations are at
the visit, where they met, where they not met.
But do our expectations align with the doctor's goals for the visit? Hmm, I
don't know. Well, what's interesting about this today is that we do have
Dr. Kim to give some insight on his perspectives, knowing he's one
doctor. So he will give some insights on that. But we also have Jerik,
and Jerik is conducting some participating in, what should I say?
Participating and leading, what's the right word?
[00:07:14] Jerik: Conducting.
[00:07:15] Tiffany: Conducting. So Jerik is conducting research into this
very topic. So not only do we have a conversation going, but we have
some research to back it up. And we know all of you doctors listening
out there like that a lot.
[00:07:30] Jerik: Mm hmm. Yeah, so I think the the framing of this
podcast actually hits on the point of the exact point that we saw is that
the kind of the expectation or the goals of the patient didn't always align
with the goals or expectations of the physician or that whoever's treating
whoever whatever type of health care provider you're seeing for your
condition. And so, you know, it could be, it's one of the more common
things that we heard was specifically about medications and side effects.
So, if I'm a patient, I'm saying that I, I, you know, I'm coming in for a
three month follow up after a medication change. And I'm telling the
physician that, you know, I've had stomach issues or I've had food
sensitivities since I started on this medication.
But the physician might tell you, hey, that's not supposed to happen. I
don't know why that's happening. Or they'll say like, you know, that's not
supposed to happen or move on or something like that, that, that specific
interaction is kind of encapsulates what we heard.
[00:08:32] Kelly: That's the main, the main crux.
[00:08:34] Tiffany: The other thing about this is when we're talking about
going into the offices, we hear a lot of things online, and so it could be,
well, I did this medication and it worked, or, you know, I tried this and it
worked, or my Rheumy does this and my Rheumy, so we hear a lot, and
I think we carry what we hear from other people living with these diseases to the office as well, and I think all of that is a, is our stepping
stones to breaking open the discussion about our expectations, the
rheumatology expectations. And if we don't understand those going in,
how are we really going to solve the entire problem of communication?
So, in saying that, I know myself, as a person living with these diseases,
I've, Dr. Kim is my rheumatologist. See, but I sought him out. Yes. So I
had a lot of trouble getting a diagnosis originally back in 2009 is when I
got my first diagnosis.
But then after that, I moved to Phoenix and it all started over. And and
then that's when I, I was rediagnosed with non radiographic axial
spondyloarthritis in the first place. But then I moved to St. Louis and I did
something foolish. People out there living with these diseases, you
should never do this.
I didn't research my doctor and I just went with what it, why insurance
provider suggested and she ended up telling me there's nothing wrong
with me, refused my medication and I started flaring tremendously.
Needless to say, I did walk out of that office and then I started
researching and I found Dr. Kim. So I hand picked him and I remember I
had to apply and he had to accept me and I don't know, are, are, are
you, are you having regrets now?
[00:10:30] Dr Kim: No comment. No, I'm joking. It's wonderful to have
you actually.
[00:10:35] Tiffany: So as we, we toggle this into the, the rheumatology
offices, I'm just curious, we, you know, we've talked a little bit about what
patients expect and we'll, we'll circle back with that, but Dr. Kim, you
know, what, what do, what are the doctor's expectations? Dr. When
seeing a patient, I know it varies if they're a new patient versus if you've
seen them a while or the, the variation of, of their disease. So it's kind of
a loaded question, but what are your thoughts about the expectations of
rheumatologists in general?
What do you, what are your goals when, when we leave that visit?
[00:11:09] Dr Kim: Right. So I think the most important goal for us is to
determine what's actionable, right? So is the information that we
obtained from you during the medical interview and the physical exam
sufficient to be able to then say, okay, there are certain laboratory tests
that we need to order?
Are there imaging studies, or are there other studies that need to be
done in order to either support or rule out certain diagnoses? So we
think of this as a very medical thing. And in preparation for this, we do,
the most important thing we do is review other physician records that
have been sent to us.
And I think you used a phrase, starting over, which is very Tiffany,
because this is very common. I think that, especially in Rheumatology,
Rheumatology is kind of a unique discipline in the sense that, to me, it's
like psychiatry. There's no lab test for bipolar disease. There's no lab test
for depression.
There's no lab test for anxiety. These are clinical diagnoses. Virtually all
of the diagnoses in Rheumatology are also clinical. But, what ends up
happening is that a lot of physicians over interpret the meaning of a
positive test. If you're a positive ANA, they say, Oh, you tested positive
for lupus.
Actually, that is, that actually sets the patient up for a potential conflict
with the next provider that sees them that's trying to interpret what that
positive ANA means. Right. So for me, I think the most important thing,
and this is true for all physicians, is that reviewing the medical record
gives us an idea of, okay, what can we, what are we pretty sure of?
What do I need to confirm in the visit? What is, and for me, and I guess
everyone may be different, I'm trying to also understand what could be
the potential mindsets. of the patient as we start discussing the
possibility that a certain diagnosis may not be right, or if the patient
doesn't feel like they have that diagnosis, it actually may be right.
And so we have to make sure that we're prepared for that conversation.
Right. But to do this, the extent of starting over is, I think this is very
frustrating for patients because you seem like you're answering the
same questions over and over and over again. But a lot of this is making
sure that the physician actually put it in the record right the first time and
this doesn't happen. All the time. Right?
[00:13:33] Tiffany: No, it doesn't. And it, one of the very interesting
things, I know Kelly, you had mentioned that one of the expectations of
going into the doctor's office is strongly based on treatments often and
getting on the right treatments. And I know for myself that there has been situations where to get the medication that is best for me or
deemed would be best for me or has worked best for me.
There's been changing to say, oh, well, you might have to put on
rheumatoid arthritis in order to get access to that. And when that
happens, my charts go to the next doctor and then it doesn't have the
right diagnosis on it. And that is happening a lot as well. So this whole
idea that and I don't know, maybe you could weigh in on this a little bit,
Dr. Kim, one of the things that patients have mentioned is that, well, my
rheumatologist say it doesn't matter what treatment you're on because
it's all, they're all treated the same, you know, you're always going to
start on X biologic or, you know, a DMART or whatever the journey is,
but it doesn't really matter because it's all the same.
So it doesn't matter what I necessarily diagnose you with. Well, just get
you a diagnosis. We hear that a lot. And what are, what are your
thoughts on that? Because it, it, our interpretation, patients feel that a
true diagnosis is very important. So could you, do you have any thoughts
on, on that as far as that's our expectation?
[00:15:07] Dr Kim: I think for 99 percent of diseases that are out there
the diagnosis is critically important in rheumatology I think what's really
strange and this took me a while for me to accept as a trainee as a
fellow here is that the symptoms are actually supersede the diagnosis in
the sense that if you have inflammatory arthritic pain so in an
autoimmune etiology for arthritis pain say in your fingers regardless of
what the diagnosis is, the treatment actually is relatively the same.
And what's strange about our conditions is that I think we still practice,
because we don't have the laboratory tests to give us the granularity to
be able to understand that a certain symptom is because of a certain
disease. All we can do is say, okay, their symptoms are consistent with
an inflammatory arthritis.
That's most likely autoimmune in origin. We've confirmed with some lab
tests and we've confirmed with some radiographs. And regardless of that
underlying diagnosis, it gets treated the same. Now, I don't think
physicians do a good job of explaining that to their patients. Again, going
back to communication.
[00:16:15] Tiffany: Communication, right.
[00:16:16] Dr Kim: But, you know, this is the real issue and we can go
into kind of the barriers for this later. But this is the single, probably most
big, the biggest complaint that we see. Actually, you know, when we first
met Tiffany going through your chart, I knew there was some incredible
utter confusion that you were experiencing.
Right? Even though we had never discussed because I was confused
too. Right? But so what ended up happening was like, I just need to
understand what symptoms we're having regardless of the diagnosis.
Right? And you really use that as the basis. And I remember when we
first talked, I was like, we met, we actually had this discussion.
I'm not sure what you're diagnosed with, but the bottom line is that you
have these symptoms and based off these symptoms, then there's
actually these medicines. So it is different than cancer, for example. The
diagnosis, the tissue, which organ, the cell type that's affected, really
important, right? But in rheumatology, we're so far from that.
So that is It's confusing. I totally get why it's confusing for patients.
[00:17:21] Tiffany: The other thing, just as a summary too, you said at
the very beginning when you were talking about when we started talking
about this topic, that the expectations of the doctors, I mean really based
on clinical, right? I mean, that makes sense.
You're the, you're the doctor. And I think that a lot of when patients walk
in, it's emotional and when you've got clinical versus emotional, those
are very different dynamics.
[00:17:47] Dr Kim: Right. So actually, I pulled up this quote by Dr.
Kenneth Robinson. So he's president and CEO of the United Way of the
Mid South.
And he actually made this comment that 80 percent of health outcomes
are determined by social determinants, 20 percent through medical care.
So social determinants, just for the audience, is essentially the variables
of how your living situation, your working situation, influences your
health. So this could be income and wealth, power that, you know, at
work, but also social support, education, employment status, addiction,
disability, all of these variables.
There's, you know, there are dozens of these that influence health. So,
physicians as classically trained, we actually don't know how to address
social determinants. We know how to address the medical aspects. So I
think this is where Dr. Robinson's quote is so, it strikes very deeply in
terms of how we execute medicine in 2020, is that we are, the
physicians are still largely stuck in that 20%, largely because that's what
we're trained in.
[00:18:54] Tiffany: Right.
[00:18:55] Dr Kim: Most clinics, and certainly me, prior to meeting Jerik,
I was totally ill prepared to deal with social determinant issues,
discrepancies, you know, disparities and that. So this is, I think kind of
one of the things I'm trying to, we're trying to fix within our own lupus
clinic is, you know, how do we address these disparities of social
determinants in order to improve outcomes?
[00:19:14] Jerik: So the, the way that I've heard a lot of people talking
about this and what I found helpful I think that what Al brought up with
the, the 80%, 20%, that's a good way to think about it. But in addition to
that, it's maybe upstream and downstream. So what the, the care that
you get from someone like Dr. Kim at a rheumatologist's office, that's
something that's very, it's proximal, it's very close to you as a patient,
there's immediate change.
But the social determinants, you can think of them more as upstream
from the health outcome because the, the care that the treatments that
you get from a doctor, there was, those are going to have like an
immediate health outcome, but fixing or addressing something that's
more upstream, it might not have immediate health outcomes, but it's
still, it's kind of like the medium by which the medium in which medical
care happens and it's be foolish to ignore it, to keep ignoring it and also
the second thing is that Dr. Kim mentioned this how do we then integrate
the concern for social determinants in the medical setting? And some
things that maybe you two are familiar with that are, I think are more
popular in rural settings and primary care is this idea of a medical home.
So, or integrated care, just something like having, having different
services that might be most necessary at a given visit that you can as a
patient, say if you have trouble, you're having trouble registering for
Medicaid or something like that, there's going to be someone on site at
your visit to help you do that.
Or if you don't have transportation, the clinic is going to facilitate your
transportation needs. Or if there's a behavioral health person on staff for
the clinic to take on, you know, what they call warm handoffs for
behavioral health, like anxiety, depression. So same care that day in the
same facility.
So that type of thing, I think, is something that the lupus clinic is, it's a
goal that the lupus clinic is probably aspiring towards, is having this
medical home type setup.
[00:21:23] Tiffany: I know, I know that that is something that, Kelly,
you've talked about in some of your blog articles too, that that is a, that is
a desire of expectations to be, to have a whole community working
together in addition to the primary conversation between the specialists,
et cetera, if you wanted to expand on that.
[00:21:42] Kelly: Sure. Well, I did have a, an experience where, you
know, I have several conditions with several different types of doctors. I
have a rheumatologist, a gynecologist endocrinologist.
So in going to all of those people, most of my doctors were in the same
medical system. My primary doctor, unfortunately, was not. So, I don't
think I realized how important it is to have that consistency of everybody
being on the same page. And, again, this is going back maybe, I don't
know, ten or more years, maybe a little less.
My blood pressure was up and my rheumatologist expressed concern
and I would go to my doctor and his physician's assistant would say, no,
it's fine. My endocrinologist was concerned and again, so it kept
happening. So prior to going on a new biologic, I knew one of the side
effects was going to be increased blood pressure, that was a risk. And
they had talked to me at my rheumatologist office about that being a risk.
As a result, I made an appointment to try and be proactive. I met with my
general practitioner's physician's assistant because I couldn't get in to
see him. And he basically said, if we put you on any more blood
pressure medicine, you will pass out.
So I, I left feeling very defeated and I left feeling sure that I was right,
that there was a problem. And I was very defeated in the sense that he
didn't hear me. But I, you know, I'm not a professional. I, I'm not a
medical doctor. I'm not a physician's assistant. So I trusted him. I had
been with the practice for a long time.
Well, the day I went in for the infusion, my blood pressure was 160 over
110. And my rheumatologist, who I swear is my angel, literally, I'm in a
building where there are several specialties, and she took me by the
hand and walked me next door to the cardiologist. Although I liked my
general practitioner, I needed everybody to be within the same system.
So having that idea of a home, I changed general practitioners. All of my
doctors are in the same system, and I'm lucky. I'm near a major city,
amazing hospitals there's teaching hospitals, so we have a lot of
research going on. We have a lot of stuff that happens in this area, so
I'm one of the lucky ones, and I'm very aware of that, but I think, you
know, like I said, if I go and tell a doctor that something's really wrong
and I end up in the hospital as a result because what I said wasn't
listened to, then you're not going to be the doctor for me.
And unfortunately, you know, I did end up in the hospital and it was a
very serious situation and I had some permanent damage from that. So
I've learned and through that, tried to express to other patients that you
really have to advocate because I think, you know, like you were saying,
there's total different, there's different expectations when a patient goes
to a doctor as opposed to when a doctor walks in.
And I think when you know, a lot of patients get nervous, there's the
whole white coat syndrome. And that's what I was told for the longest
time was the reason why my blood pressure was so high. My general
practitioner's person kept telling me, oh, you have white coat syndrome.
You just get nervous when they take your blood pressure.
So again, we've already talked a little bit about the goal that, you know,
our doctors have when we walk in versus the goal we have that we walk
in. Is there any way that we can maybe pull them together a little bit
more? Any suggestions? I know through my blog, I've written down, you
know, you go to the rheumatologist.
You might not be flaring. You look great. Your blood work looks great.
So, , along the way, I take pictures of my joints when they swell because
sometimes I can't believe how bad they are. I write down the days that I
don't feel well, I try and give her as much information as possible
because she insists I don't complain enough and I insist I'm like, oh, it's
not that bad. But yet when they see me and my joints are so big yeah, it
does get that bad. So I think that communication piece is really really
key in knowing what to sort of talk about my doctor and I I have a really good relationship. I always tell her she's never allowed to retire or leave me.
Because my last one did retire and left me and I, it was a struggle, as
Tiffany said, trying to find somebody. I also had someone who told me,
there's nothing wrong with you. And I said, oh, well, if there's nothing
wrong with me, why are all of my joints swollen and red? And he said, I
don't know. I was like okay, well you're not the doctor for me.
But again, none of us really want to have anything wrong with us. So the
talk about, you know, none of us really want a diagnosis, even though
we do want the diagnosis. We just want to know what's wrong with us.
We want to be able to explain it to other people, and I think the social
piece with friends and family is, since we can't always explain what's
wrong with us, it's hard for them to understand maybe what we need,
and I think that is a piece. Dr. Kim, do you have anything to add to that?
[00:26:36] Dr Kim: I, I think you bring up something that's really
challenging for physicians, is that, so, Particularly in psychiatry, in
rheumatology, and also other disciplines where we have to, so I think the
toughest job that we do is that we have to take the colloquial coming
from the patient, translate that to technical so that we can apply what
we've learned medically, which is taught technically.
And then translate it back to colloquial to be able to have you guys as
patients understand with the full intent of what we mean. And oftentimes
that skill is, I think, oftentimes implied that it's going to occur during
medical training. You know, I can't actually think of any work that we've
done when I was in medical school or even residency where we actually
talked about when a patient says this, what, what are you, how are you
interpreting that, right?
And I think this is also goes down to how good of a physician that he or
she is, is being able to say, you know what, I need to work with much
more granularity on what was just said in order for that piece of
information to be actionable, right? And I don't know, I don't know how
well this is done globally by physicians.
I think this is something that I sometimes see some of our, especially
young residents they just, they interpret what the patient says the way
they want it to, because their time constraints. Right. And sometimes you have to back up and say, listen, I'm not actually 100 percent sure
that's what they meant.
[00:28:10] Kelly: And I do have to say, I think the time constraint is a big
thing and that's driven more by the industry and insurance than it is by,
you know, a doctor wanting to take the time. My rheumatologist, I wait at
least 20 to 35, sometimes up to an hour to get in and I know so many
people get upset and I don't get upset because I know she's actually
listening to people and the one day she came in on time and I was like,
what's wrong?
Why are you here on time? That doesn't happen. But I don't get upset
about that because I do see that as being, she's listening and she's
taking the time to explain. And I do think, you know, as being someone
who, you know, all through school, I'll be working and I'm like, you know
what, I wasn't prepared for this in college.
I don't remember that day they mentioned that this is how you have to
explain things to a client. So it does make sense. I think there's a lot to
be said for, you know, you have to learn things. And I think the
communication piece as a speech language pathologist, I mean, that's
my area of specialty, you know, reading between the lines is a very
difficult thing.
And that patient relationship, like Tiffany said, patients tend to be more
emotional and that can make getting your stuff across very difficult.
That's why I really do recommend that patients document their concerns
along the way and almost coaching them on how to be a patient. Dr.
Kim, do you have anything else to add to that?
[00:29:30] Dr Kim: I just want to add something about the time issue
because as physician visits are being cut shorter. Right? It becomes a
lot harder to be able to extract out, you know, meaningful information
from patients sometimes because, you know, oftentimes it, it is
emotional and that needs to be expressed. All right.
But what ends up happening, especially for physicians who are deeply
empathic, is that because there's so many patients now that are seen
during a day that actually causes emotional burnout for the provider. All
right, and you know add that with em electronic medical record burnout
Right. I think you know, one of the biggest problems that we're seeing
within our industry generally is is wellness mindfulness of physicians and these are actually efforts here at WashU they're trying to actively
address is that you know if you really want to emotionally invest into a
patient, that's exhausting. But now you have to do it 20, 30 times a day,
each person coming up with different sets of complaints, or even very
similar complaints, but it manifests and impacts that patient differently.
You know, how do you maintain your energy without feeling like, you
know what, I just can't do any more today or this week. Right. So these
are system errors as you brought up, Kelly, that I don't 100 percent know
what the solution is because obviously this is a financially driven
decision.
[00:30:53] Kelly: Right. And you know, that's just one of the many
barriers that we have in terms of communication with our doctors.
And I think, you know, now my, my medical system is very much,
everything is online now. So, like I said, anything I say to my one doctor
gets translated to my next doctor. So, if my medications have changed
or anything, all of that stuff is really taken care of when I walk in and they
just sort of review things with me.
But I think what I've tried to do through my blog, I think what Tiffany and I
have done through IFAA is to really help patients, not really teach
patients how to be a better patient, but to sort of empower them with
skills that they can use to go into these situations. Because again, I
know I was lucky enough to attend the ACR, the annual event, the
Capitol Hill Day, and the one rheumatologist I went with, he is new to the
Philadelphia area.
And he's only been in practice there a few months, and he said there's
already a six month wait for new patients. And when you think about
that, that's six months of a patient not knowing what's wrong with them,
reading lots of things from Dr. Google that scare them, all those things,
you know, really add to the whole emotional component.
And I think that is a really important thing that patients have to really
understand too, that Listening to people all day long talk about being in
pain is draining. It's emotionally draining. It truly is.
[00:32:15] Jerik: Yeah, so I'll add, I think that what you just described
with the blog and trying to teach patients how, like skills, specific, like discrete skills that they can use in their doctor's appointment is really important.
And a lot of the field and the communication skills, training, and literature
focuses on this and improving communication in doctors. There's been a
lot less on patient specific skills training. It's unclear to me why exactly
because communication is a two way street and it needs two individuals,
the patient and the doctor to, to work.
And when we're talking about misalignment of goals, it's not that one,
well, patient goal should be, this should be like the most important to,
that's what I believe at least. But I think the giving patient skills to
acknowledge and also because doctors are people too and they also
want to be validated or affirmed or made their experience like relevant
and knowing that like going back to the time, like, you know, this is
maybe they're not having the best day or something like that, but that's
something that the, you know, the patient is also responsible for
addressing as well.
[00:33:27] Tiffany: No, that's, that's interesting that you said you say that
because one of our goals of this whole RheumyRounds series is so that
we can collect enough information to develop tools and resources that
solve the problems that we're talking about. And one of the things that
we do as a pillar of objectives that IFAA is to utilize our experiences as
people living with the diseases who have the opportunities to speak with
doctors who have the opportunity to go to the American College of
Rheumatology meeting or EULAR, the European League Against
Rheumatism. And then from that, in all of the information we're collecting
and inviting patients to listen to these and be part of the conversation,
then we can begin to really use our backgrounds to teach.
And, you know, Kelly has educational background. I was a college
teacher for eight years, several people who are on affiliated with, with
our organization have backgrounds in teaching. So it's, we hope that that
becomes a reality. That's part of this goal. But the bigger overarching
goal of RheumyRounds, as we said in the beginning, was really to open
up the communication lines between doctors and patient so that we can
address issues that both stakeholder parties are talking about. So, you
know, patients talk to patients. And from that, we at IFAA have been
able to identify some key issues. And some key communication barriers,
right, between what patients are expressing in this particular topic.
Again, it's on office visits and doctors are talking to doctors, but we
cannot solve the problems that exist between the communications if we
do not put all parties at the same table to have a. heartfelt discussion so
we can understand what the other person, what the other, the other
stakeholder group is, is feeling dealing with.
So I'd like to thank Dr. Kim, Jerik, and Kelly, as we come all, we all come
to the table and we're inviting you. So pull up a chair. It's time to have
your voice heard. AiArthritis Voices 360 is produced by the International
Foundation for Autoimmune and Autoinflammatory Arthritis.
Find us on the web at www. Airthritis.Org. Also, be sure to subscribe to
this podcast and stay up to date on all the latest AiArthritis news and
events.