[00:00:00] Tiffany: Welcome to AiArthritis Voices 360, the podcast
solving today's most pressing issues in the AiArthritis community. We
invite you all to the table where together we face the daily challenges of
autoimmune and autoinflammatory arthritis. Join our fellow patient co
hosts as they lead discussions in the patient community, as well as
consult with stakeholders worldwide to solve the problems that matter
most.
Whether you are a loved one, a professional working in the field, or a
person diagnosed with an AiArthritis disease, this podcast is for you. So
pull up a chair and take a seat at the table.
Welcome to AiArthritis Voices 360. This is the official talk show for the
International Foundation for Autoimmune Autoinflammatory Arthritis or
just AiArthritis for short. My name is Tiffany Westridge-Robertson. I'm
the CEO of the organization, but also a person living with diseases as
most of the people of our leadership and our organization and the co
hosts that I have on with me today.
So my diagnosis is non radiographic axial spondyloarthritis. And I'm
excited, excited, excited about my co host and the topic today. So let's
meet those co hosts I keep raving about. Oh, welcome back Danielle!
[00:01:32] Danielle: Thanks Tiffany. I'm glad to be back.
[00:01:34] Tiffany: All right. So did y'all call everyone a little bit about
you?
[00:01:38] Danielle: I'm a volunteer for AiArthritis. I've been on leave for
quite a while for pregnancy and postpartum and most recently a hip
replacement. So I'm very excited to be back. I am also on the board of
directors for a social justice organization called Ride the Omnibus. And
I'm very excited about this topic and to be here with you guys today.
[00:02:02] Tiffany: Hi. And Ms. Kerry.
[00:02:05] Kerry: Hi, everyone. I am Kerry, as Tiffany said also known
as the butterfly from FloatLikeAButtahfly. I am a writer and patient
advocate doing a lot with AiArthritis and a couple other organizations as
well. And I am also a person living with a long list of these diseases too.
[00:02:25] Tiffany: So you had a lot of different diagnoses. So they're
like, I got to be on this episode. And what is the topic and the burning
question of the day? Why can't I get diagnosed?! So this is a topic that I
can't believe we haven't actually put this one on the table yet. We've
talked about other things. We've talked about the mystery patient, you
know, we have sort of skirted around it, but we're getting right to the
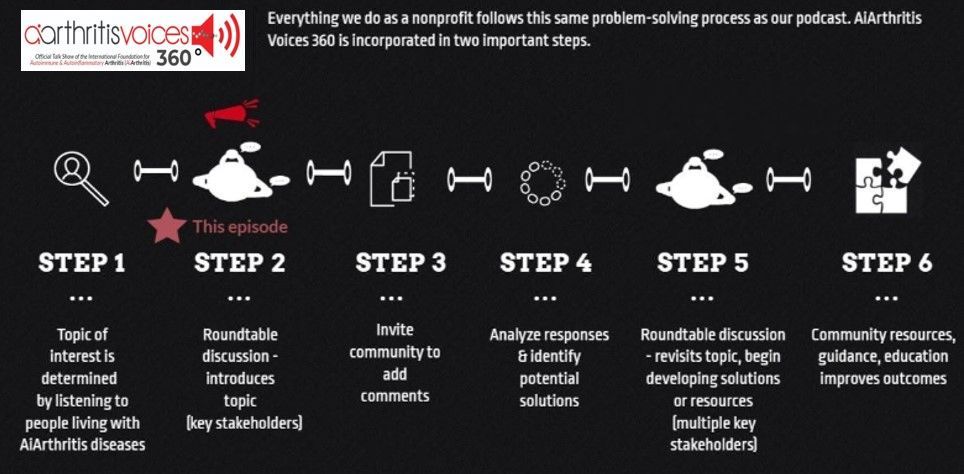
point today and one of the things that you may or may not know about
AiArthritis is everything we do at our organization, every project we bring
on that we tackle is based on what patients tell us is most needed. And
so we look around and we see what other resources are out there.
We won't duplicate efforts and then we figure out if there's anything
missing and we try to create innovative ways based on what patients say
and we create these resources. So they're literally patient led resources
and we say patient infused pun intended solutions. So we're going to
start talking about a way that we can talk about this issue.
Why can't I get diagnosed? Why can't you get diagnosed? It's a number
1 question that comes into our organization. And we represent people
diagnosed like myself, Danielle, Kerry, we represent support network,
your family, your friends, your, your loved ones, but we also represent
the undiagnosed. So undiagnosed, this show is for you.
We are here for you because we've all been through this before. So we
really just thought we would dive right in with patient stories, we all here
have a story, you have a story, Kerry has a story, Danielle has a story, I
have a story, they have multiple diagnoses, they have many stories, but
the point being, it's frustrating when we don't have any answers, right?
So I'm going to turn it over. Danielle, did you want to start with just a little
bit of why you really wanted to be part of this episode?
[00:04:30] Danielle: Yeah, sure. Absolutely. So one of the first things
I've noticed patients talk about when we get together is like how long it
took you to get diagnosed. And I had my very first symptom that looking
back, I now know was part of my disease when I was eight years old and
I wasn't diagnosed until I was 36. So that usually gets people like what,
how did that happen? And how did that happen is a story that has had a
profound effect on my life. You know, being ignored and having doctors
not listen to me and by the time I actually got a diagnosis, I was in a
wheelchair.
So this topic is super important to me because nobody should have to
wait that long. I mean, I think once I heard on the show, the average
time is about 10 years or something like that and that's way too long.
You know, frankly, when you're in pain, one year is too long. Like we
have to get better at this.
[00:05:32] Tiffany: Yeah. Yeah. And some of the diseases. that are
more common or which we'll talk about a little bit in our breakout
conversations, a little bit easier to diagnose might take less time. So for
example, rheumatoid arthritis, one of the ones that have the one to three
year range for diagnosis, and you'll hear people diagnosed a lot quicker
with that.
I'm not a medical professional. And I do want to preface that with out
with all of us on the show. These are our opinions. These are our
perspectives as lived experience. Okay. So my theory, my perspective
here is as a person originally the mystery patient, then the
undifferentiated connective disease patient, which by the way, at the
time I felt was not a diagnosis, but I know now it is a diagnosis and then
eventually rheumatoid arthritis. Then changed from rheumatoid arthritis
4 years later to non radiographic axial spondyloarthritis because there
was no such thing as my diagnosis, so it wasn't a misdiagnosis. But my
point in saying that is, I fell into the 3 year with rheumatoid arthritis, but I
didn't have realistically, I don't meet the statistic, but I also point that out
because it is one of the easiest diagnoses of all of our diseases.
It doesn't have a stringent criteria to be diagnosed.
So I'll, I'll, I'll stop
there on that. And we'll revisit this topic as we move forward. But Kerry, I
know when you could probably spend the whole time talking about your
diagnosis journey but we're gonna, we're gonna crop it a little bit. So
what are the main things that you want to tell us about with this
diagnosis story?
[00:07:29] Kerry: I definitely, as soon as I saw that you were coming out
with this as a topic, I jumped through my computer to say please book
me on this show because in the super short version, it took me eight
years to get an accurate diagnosis, but that includes so many years of
being dismissed just because I didn't look sick and there was no need to
even look any further.
And then another four years of rotating diagnoses, so kind of the way
Tiffany you had it was non radiographic axial spondyloarthritis. We
actually thought that was one of mine too. I also didn't know at the time
that undifferentiated was a real diagnosis. I thought that, and the way it
was explained to me, was It means we kind of sort of know that there's
something but it hasn't yet fully developed into one of the other real
diagnoses.
And I went through a slew of it kind of sort of looks like lupus, but so let's
try this medication. Oh, but no, it's not. And it kind of sort of looks like RA
but it doesn't have the rheumatoid factor. It kind of, sort of looks like
stills. It kind of, sort of looks like four years worth of what it kind of, sort
of looked like before we could figure out what it actually was.
And of course, along that way, things got worse. You know, there was a
lot more damage being done, disease being progressed, and even
additional conditions that kind of grew alongside it. So this is such an
important topic because it really hits home so much for me, but because
I know it hits home for so many people out there watching or listening.
[00:09:23] Tiffany: Absolutely. I think one of the quotes that I just wrote
down that you said that I think we all can relate to is things got worse.
And that's such an important point as we're pulling out some important
factors on the why we need to get this message out and why we need to
help the undiagnosed get some answers is because there is a window of
opportunity.
For our diseases, the American College of Rheumatology and EULAR,
which is the European version of the scientific groups that determine the
criteria for diagnosis and treatment protocols and such they recommend
treatment start 6 months after onset, which it's hard to even get into a
rheumatologist in 6 months if you're a new patient.
So that alone, that's, that's what we call a 360it, where we go off and we
can talk about access and, and what leads up to some of these, which
we will definitely branch off into several of these topics in the future.
[00:10:27] Danielle: That also assumes that you know you need to see
a rheumatologist. I saw seven orthopedists before I ended up at a
rheumatologist.
[00:10:35] Tiffany: Yes. Let's actually, let's actually break off right into
that Danielle, because when we were previewing what we were going to
talk about on the show, you talked specifically about this and I think that
it leads into this bullet. We've got the window of opportunity that we're
supposed to hit and the reason why is because research shows and
we're seeing it every time we take, we go to the ACR. Every time we go
to EULAR we're seeing the word remission and we're like, and remission
is happening to the people who are getting the diagnosis early, who are
getting the treatments early, which is why this is so important.
But that's not the norm. It's not the norm. And too often we get a detour
on our road. That is one of these main issues of why we're not getting
diagnosed. So Danielle, why don't you talk a little bit about that?
[00:11:28] Danielle: So I think that that really breaks into two parts. First
of all, as a patient, you have to know that you need help.
And for me, that was a huge hurdle. And at the beginning of my journey,
I was a kid, I didn't know anything. But even if you just limit it to when I
was an adult, and I was going to see my own doctors you only have ever
existed in your body. You don't know what other people's reality is like.
So I thought everybody had chronic pain.
I thought everybody was tired all the time. I thought everybody had
random fevers that popped up out of nowhere like I didn't know that was
unusual. That was the first thing. And then when I did start asking for
help, my doctors would go, Oh, there's something wrong with your
shoulder. Go see an orthopedist.
There's something wrong with your knee, go see an orthopedist. Nobody
sent me to a rheumatologist for years and years and years. And in point
of fact, when I did finally end up at a rheumatologist, it's because a
radiologist came back and said look, I pulled this patient's MRIs for the
last three years and I think this is RA. And that's when an orthopedist
finally sent me to a rheumatologist. So even just recognizing that I
needed to see one was a huge problem. And then the other part of it is
once you know that you need to see a doctor and you're sitting in front of
one, getting them to listen to you can be a huge problem. You know,
most of the people who take a long time to get diagnosed like you guys
have zero negative versions of things. And I know we're going to talk
about blood work here in a bit, I, that wasn't me when they did finally test
my blood. I had rheumatoid factor positive. I was ACPA-positive.
I mean, my blood work was screaming this person has a rheumatic
disease, but nobody ever tested it that whole time. So. We know that
some members of the medical community have bias that they're not
aware of and they tend to downplay women's pain and like 90 percent of
people with rheumatic disease are women.
They tend to downplay pain from people of color. They tend to downplay
pain from children and when I first started saying, I don't think I can walk
if you don't do something about my knees. I was 14. I was, and to me
now, this is crazy, but I was given prescription strength arthritis
medicine. It was called Vioxx.
It's not on the market anymore. When I was 14 years old, but nobody
thought maybe we should test her blood work like it's weird for a kid to
have this much pain, but I think they gave me that script to shut me up
because they thought that I was making it up or they thought I was
exaggerating it or something like that.
So getting a doctor to listen to you can be a huge hurdle. If anybody had
bothered to order a test, they would have found it right away because it
wasn't hiding. But, you know, nobody did. And the other thing that I
heard a lot of was doctors who wanted to put stipulations on treatment or
even on investigations.
So they would tell me things like, well, I want you to try a vegan diet and
then come back and see me if it doesn't go away. I think you might have
food allergies. Let's try elimination diet and then come back and see me
if it doesn't go away. Probably you need to exercise more. I even had
one guy tell me that women's anatomy was more prone to muscular
dysfunction and I should try yoga and then come back and see me if it
doesn't go away. As my disease progressed and I became less and less
mobile, then it started being about my weight. Well, lose 10 pounds and
then come back if you're still hurting. You know, none of that should
have ever happened.
The minute I showed up in their office and said, I am 16 years old, I'm 23
years old, I'm 31 years old, and I am in pain all the time. They should
have ordered tests. They should have ordered imaging. You know, we
shouldn't have to beg for someone's attention.
[00:15:41] Tiffany: Kerry, you're, you're, I could just see it. You're right.
You're like, ah, go for it.
[00:15:47] Kerry: So much of everything that you said, Danielle, I just
feel so much. And so I want to start with that first thing of, we have to
know that we even need help. And how much we don't realize is actually
a problem because now I said earlier, it took me eight years to get an
accurate diagnosis.
That's eight years from when I started trying to get one eight years from
when I said, Hey, I think there's something wrong. We really need to look
at this. But when I think back, you know, and I've, I've talked about this
before, you know, I used to say I always had a bunch of what I called
random achy pains.
They didn't belong to anything. They weren't associated with anything.
They weren't for any reason. I just hurt in different places at different
times for no reason. And I thought that was just life. I was just at an
arthritis conference and I heard from so many other patients who said
the same thing.
They were children and they were told, Oh, this is growing, you know. I
was then, you know, later on, even once we got to a point where the
doctors finally said, Okay, yeah, maybe there is something wrong with
you. They weren't very interested in finding out what, and it took until
there was something completely undeniable, you know, four years of me
telling them about my pain, my fatigue, my, you know, struggles with
dizziness with balance, you know, all of those things that didn't mean
anything because it didn't show up on a lab report.
It was only when after four years of saying doctor, please help me, to a
whole lot of doctors, it was only then when my feet swelled up so big that
I couldn't put shoes on that I said look, I am not making this up.
Depression didn't do this. And that's when they finally said, okay, you
have some kind of arthritis.
It's probably autoimmune. Here's some steroids and have a nice day.
And then, you know, he had no interest in doing anything further than
that. He didn't tell me how dangerous steroids could be while they are
helping with certain things, they are seriously hurting with others. I know
you mentioned earlier that, you know, you just got the hip replacement.
So did I just a few months ago. And the primary reason, I mean, I have
as my rheumatologist calls it a little bit of RA I have a little bit of
Sjogrens, I have a little bit of other inflammatory things. My primary
diagnosis is a rare inflammatory disease called sarcoidosis. That is also
cause musculoskeletal sarcoidosis or or sarcoid arthritis.
But the primary reason what got so far beyond bearable was that I
developed osteoarthritis and a vascular necrosis and for anyone who's
not who isn't aware a vascular necrosis is basically when your bone
begins to die because it's not getting the blood or the oxygen that it
needs to survive and the reason that happens long term steroid use and
osteoarthritis and what's one of the big causes for osteoarthritis?
Well, what steroids do is they, you know, one of the side effects is
excessive weight gain. I gained over a hundred pounds, but at the same
time as it makes you gain weight, it also makes your bones weaker.
That's a really bad combination. And if I had gotten a proper diagnosis
earlier. I would have gotten proper treatment earlier.
And as much as I love my new hip right now, I might not have needed it
if I was able to get diagnosed when I should have been.
[00:19:38] Tiffany: Absolutely, looking at notes that we all take before
we start and the growing pains for the kids. And, you know, we've all
heard, oh, well, we talked about, you must be depressed or I got
well, you obviously hurt yourself at the gym because I was an athlete
and I kickboxed and I played sports and even they didn't believe my
inflammation for a couple of reasons. Well, my blood work was negative,
so we'll break out here and start talking about that. And I was very, very
thin, muscular, athletic, and I knew that I couldn't fit my foot hurt inside
my shoe.
I knew that my foot was swollen because I couldn't tie it in my shoe. It
wasn't fitting correctly, but visibly they weren't seeing it like I said, I was
very, very thin and bony and it probably just looked normal. I was telling
them that I couldn't put my shoe on and that wasn't registering because I
didn't have any clinical measurable presentation that they could find and
so one of the things that we will talk about in a continued conversation
with this is a little preview is there's going to be a continued conversation
here next month on the next continued discussion of this on our
RheumyRounds episode where we're going to be talking to
rheumatologists, bring them to the table, ask them why we don't get
diagnosed and see what advice they can give, but one of the top
reasons is your blood work looks fine. So we are going, that's going to
actually be the main theme of the next show. And I want to really bring
this point up because to be diagnosed with some of our diseases,
including rheumatoid arthritis, you do not need positive blood work, do
not need it.
So all of the people out there who are messaging AiArthritis or talking to
each other or talking to family members or whatever, you hear
somebody say well, the good news is I don't have RA because my blood
work looked fine is a false statement. If you take nothing from this
episode today that does not mean you don't have rheumatoid arthritis.
Okay. So it can mean that you have worser disease because that is
proof. Research has shown, Danielle, you mentioned you were at ACPA
positive, rheumatoid factor positive. You don't need those to have
rheumatoid, even though it's in the name. You don't have to have those
to have, people can have rheumatoid factor positive and not have any of
our diseases.
It's a blood marker. In saying that, people with our diseases that do have
these markers have typically worse outcomes, meaning they have more
aggressive disease, they might be more difficult to treat, they might have
worse flares, that type of thing. And so that's also slinging back why I
realized in the beginning undifferentiated at sometimes, not always,
sometimes it is a question mark, but also other times it can mean that
you have milder onset, which if you snip it and you get treatment for it,
that is actually could be a good thing. And my journey undifferentiated
why Kerry, I feel that I thought it was a bad thing was because they told
me similar to what you were told.
I can't treat you is what they told me. I can't treat you until I can figure
out what this grows into, what this becomes a full fledged disease. So
they were basically telling me, you don't actually have something. You
have something that is not treatable. But once I got educated, I went
back and realized there was treatment guidelines, not great ones.
But there were guidelines that said I should have been treated with
some mild disease modifying agent.
And I was denied that, and guess
what? I got worse. Things got worse, a lot worse. And I do look back a
lot today and say, I wonder if there were people like Danielle, like you
Kerry, like me, like a lot of us here at AiArthritis, like the people that you
were just at the conference with, Kerry, our friends, the people we talked
to, if we could unite and create some kind of guide, some kind of
navigation, something for these people who are coming into AiArthritis
and saying, I don't have answers, we've got to start somewhere.
And I feel like, why not start with the people who are the experts, right?
And that is us. All right, Danielle, what do you specifically still want to put
on the table here as a point that we talked about that we would bring up
that we haven't gotten to yet?
[00:24:44] Danielle: One of the things I think it's really important for
everybody who is still searching for a diagnosis to understand is that
your blood work is not a blueprint to your body. It's not something that's
static. It changes all the time. It is one snapshot in time. I have tracked
my markers now because my rheumatologist keeps changing my
diagnosis every time I turn around for several years. I have had times
where my rheumatoid factor was barely positive.
I've had times where it was very positive. I've had times where my ACPA
was off the charts. I've had times where it was fairly moderate. If you
look at said rate, which is a sort of a generic marker that indicates how
much inflammation is in your body, but a lot of doctors put a ton of
weight on that. I have had times where it was normal.
I have had times where it was 110 and normal is like less than 10. The
pathology report that I got back that time said, you know, evaluate this
patient for cancer because those levels usually indicate something
really, really bad. So just because you get back negative blood work
doesn't necessarily mean even that you're seronegative.
It may just mean you didn't have positive markers that day. Now,
obviously, if you've had multiple tests and they're still negative, that also
doesn't mean that you don't have one of these diseases. But I think it's
really important for everybody to know that one test doesn't prove
anything, and it doesn't disprove anything.
My ANA, which is also a big marker that people put weight on in the
rheumatology field, has never been positive. Not once. Which always
doctors look at me like how did that happen because that usually turns
positive before anything else, but mine never did. And the other thing
that I want people to remember is, and I think this is where we really
need to develop some kind of guide for people is that just because your
doctor tells you, well, I tested for rheumatoid arthritis or I tested for
Sjogren's or whatever, you don't have it
doesn't necessarily mean that they ordered every single test that they
should have. You know, I was told multiple times that oh well, I ordered x
rays and I didn't see anything, that means there's no damage. No, it
doesn't, because you may have damage that's only visible on an MRI at
this point. One of the big symptoms of my disease is bone marrow
edema.
It does not show on any x ray, but it is crippling and painful and very
visible on an MRI.
So we really need to be able to give patients something that they can
compare to their test results, compare to their blood work and go, okay,
they tested this and this and this. Oh, but they didn't test this. I need to
ask about it. Or, you know, I need to advocate for myself because if you
think that you're going to walk into a rheumatologist office and they're
going to order everything and diagnose you on the spot, I'm really sorry,
but you're probably not correct.
[00:27:54] Tiffany: That is such a relevant topic again, we're going to
spin off on a 360it on this because this is very relevant in what's
happening also in legislative and public policy and access to our
treatment is biomarkers and precision medicine. And so one of the
things I've been told too is you don't have this biomarker, which is a
measurement of the molecules in your blood and your urine and your
tissues.
It's part of your DNA, your RNA. And there are some great biomarkers
that can help with diagnosis. Sjogren's is one of them. I was tested for
Sjogren's. I didn't have the biomarkers, so I literally was dismissed, it
cannot be Sjogren's. However, we know now only 60 percent of people
living with Sjogren's have the biomarkers.
So that is a great tool to help confirm some, but it does not mean that I
don't have Sjogrens and to be frank, I'm pretty sure I do.
So in saying
that it's important to understand. I love that point, Danielle, and how long
the biomarkers like, there was a lot of push for getting the, what they call
full panel access.
Because what happens is your doctor will order one or two or a couple
of blood tests. And we'll just, and what could actually happen if we had
access to a full panel instead of a one off or whatever, which is only
given a lot of times for money reasons, because it only costs 40 and per
se to say a $1000 for the insurance companies, but access to it could
answer a lot of questions.
A lot of questions, not only diagnosis on what is there identifying more of
these biomarkers. But it also could help start matching us to treatment
quicker so we don't have the trial and error, which is critical, especially
for those of us who missed that window of opportunity. So that's just my
own little precision medicine rant that I had to have there.
And the other point I do want to bring up two of them that you said, I
want to reiterate x rays x rays are diseases, unless there's something
super progressive, or it just went unnoticed like you both said, I didn't
realize I had onset. It takes approximately 10 years for anything to show
up on an x ray.
So if you have an x ray and they say, nothing's wrong with you because
that happened to me too, 30 x rays all over my body when I had
undifferentiated disease and they said see there's nothing wrong
because nothing came back on the x ray. It wasn't, it was only until I
went to my second rheumatologist where he took an MRI and they
actually found some inflammation of my wrist and then he pulled up my x
ray from the same shot and she pointed at this little thing and he said,
that little bitty thing right there that actually is information, but people
don't know to look for it.
That actually is something that looks like a cyst or something. Anyway,
great point. Kerry, what else do you want to add?
[00:30:58] Kerry: Yeah, so the thing that I think sort of builds off of what
you were both saying is, you know, in not only Is it important to know
what different tests mean or what they don't mean? What tests we might
want to ask our doctors for?
But I think something else that is just so, so, so important is actually
seeing the doctor, how much the doctor actually cares to look into
things, how much they actually know about what's going on, how much
they are willing to look further into it or learn more about it or admit that
they might not know something because I will just say, you know, the,
the big difference, I have seen a lot, a lot, a lot, a lot of doctors over the
past 15 years.
And I have, you know, as I said earlier, I had some who just looked at
me and said, I must be depressed. And anybody who knows me would
say that's one of the last words they would ever think, but especially not
when I'm coming in saying I have pain and fatigue, et cetera. So there
are some doctors who will just dismiss you outright.
There are some doctors who will be content to say it's some kind of
arthritis and that's, you know, that's all you need to know. And then there
are doctors like my current rheumatologist who I absolutely love. I
actually wrote a column about her and it was called, I fell in love with my
doctor when she ordered 19 vials of blood on my first visit.
Because that showed so much, you know, I don't know if it's a full panel,
but I know she tested a lot. I know she tested a lot more than anybody
else ever did. And one of the problems I had early on with, or not as
early, but once I, in 2015, we figured out that I had this rare disease
called sarcoidosis.
Because it's a rare disease, most of my doctors knew nothing about it.
And so that became the really easy answer for everything and nothing. If
I said, I have this new pain. Oh, well, you know, it's sarcoidosis.
Sarcoidosis does that. If I say I'm having this new problem and I think it
might be sarcoidosis, because I've been reading up on it.
I got after who doesn't know any better says, no, I don't think so and they
actually leave it at that. Either, you know, they just dismiss it as it's
sarcoidosis and you already know that, so we don't have to worry about
it, or they don't bother thinking of it and don't even consider the
possibility.
Either way, they're not actually looking at me, they're not actually
listening to me, to the things that I'm telling them, to what I am
experiencing, and until I got someone who actually would do that, It was
really just delay on top of delay, disease progression on top of disease
progression and missing things left and right, you know, now I am just,
I'm so happy.
I love this doctor. My rheumatologist now is wonderful. My orthopedic
surgeon, I absolutely adore him. He's my best friend now. He's my
husband's best friend now because he gave us back something that I
had lost so long ago that I never should have lost in the first place. And
so the thing that I, you know, I know that we can go on and you will have
plenty of other conversations with doctors about doctors, what we need
and what we don't and all of that.
But the one thing that I will say to every single person who is watching,
who is listening, who is going to hear about this conversation later is
trust your gut when it comes to your doctors. I mean, with your body too,
when you feel like something is wrong. Don't let some doctor, just
because he has a degree on you, will tell you that there's nothing
happening.
You know when there's something going on. You need to keep pushing
until you get the answers you deserve. And that means you might need
to change to another doctor. Because without all of those proper
diagnoses, proper tests, proper treatments, in addition to all the physical
progression that we have, there is everything that it does to us
emotionally.
There's everything that it does to our family, to our co workers, to
whether or not we can work, to everyone who sees what we're going
through. Some might believe the doctor and think that we're just, you
know, really being melodramatic. Some might get frustrated with us
about the doctor who won't listen but it has affected their lives too. And
so, this spirals in so many different directions and so far and so wide.
And so, finding the right doctor for you is just one of the most important
things that you can do as you're trying to move forward with this.
[00:35:46] Danielle: And can I just add also, avoid the wrong ones. If
you know someone doesn't click with you, if you know they're not
listening to you, if you know that they're combative when you try to ask
for things, essentially if they're not on board with shared decision
making, you need to leave.
Because the minute they diagnose you with some kind of psychological
cause or they put something in there that you're drug seeking or
anything like that. Every doctor you have after that is going to look at you
with skepticism and it can cause some very serious damage. I've seen it
happen.
[00:36:21] Kerry: Definitely.
[00:36:21] Tiffany: Great point, Danielle. Kerry, did you want to add to
that?
[00:36:24] Kerry: That's part of that really trusting your gut. If you go into
a doctor and they don't want to listen to you, they want to dismiss you
too quickly. They don't want to look at the information that you've
brought with them, because it is important to bring information with you.
If they are dismissive in any way, you don't owe them Oh, well, let me
see them a couple more times and see, maybe they'll get better. You
don't owe them anything. You owe yourself the chance to get the best
care and the best treatment that you can and so you can walk out of that
office in the middle of an appointment.
You can make it a point to never come back again, because the one
who matters in all of this is you.
[00:37:07] Tiffany: Very well put in saying that we're going to start
wrapping it up here and definitely a 360it that we're going to have to spin
off into a conversation is when to fire your doctor, which I wrote down
based on what was just said there, which is something that sometimes
you just need to do, especially if you're looking for a diagnosis and
you're not getting any answers. It doesn't necessarily mean you may not
have an AiArthritis disease, but if you do, we cannot express enough the
importance of an early diagnosis, getting on the right treatment, not
getting thrown steroids or getting thrown something else, or going to go
to a different doctor before you get to the doctor that really could
diagnosing all of these things that we sort of touched on.
The other thing I just wanted to circle back quickly, just to mention here,
you talked about, well, it must be your sarcoidosis. And that is a very
good segment into a future episode that we are going to build on
whatever tool we start to create here for those undiagnosed. We're going
to also build on a tool for what happens when you're, you are just
diagnosed and what happens when you have a diagnosis and you're
developing comorbidities because that happens way too often.
It must be this that happened. I will do my own 360it on how something
that detrimental can happen because it was blamed on me having
Bouchette's disease. When I actually had Stevens Johnson syndrome, it
almost killed me. So that is a 360it in itself and a reason why you cannot
always, so we need an episode on that.
We are going to wrap this conversation up here, but it's not over. This is
just us putting the topic on the table. There is so much to say about this.
Because everybody is undiagnosed before they're diagnosed. So
whether you have a diagnosis or whether you're going through this, or
like you said, curate affects everybody.
If you're a person who went through this, I know my parents, you know,
they, they were so frustrated. Nobody knew what was wrong with their
child. Didn't know I was very much an adult, but I'm still their baby, right?
And all of the other aspects that come with this, there's so much to say.
This is a huge topic.
So we want to hear from you. We want to hear if you're going through
this, what do you need from us? What is your story? What are your
challenges right now? So that we can create the best resources and the
best tools. Everybody who has a diagnosis, you've been there. So what,
what do you recall? What kind of advice like Danielle's giving, like
Kerry's giving, like I'm giving, what should we add to this list?
We're going to have, by the time this airs, we'll at least have this laid out
and organized in some of the things that we've said today, and then we'll
have a form for you to submit your voice. Very important. We hope that
everybody helps unite and build this tool for those who deserve a
diagnosis in saying that I'm going to thank Danielle and Kerry for joining
me, and I'm going to ask each of you to let everyone know where they
can find you. So I'm going to start with Kerry.
[00:40:21] Kerry: Okay. Hey, everyone. So as I said earlier, my, I go by
buttahfly and I have a, you can find me at Float Like A Buttahfly on my,
that would be my website and my Facebook page and my column at
sarcoidos news, or you can find me everywhere else on social media
@ButtahflyK one quick note that I will make is a quick spelling note.
I am from New York and I say it I spell it the way we say it. It's like butter.
So it's B U T T A H fly. So that's float like a buttahfly or @Buttahflyk
either one.
[00:40:56] Tiffany: All right. And Danielle?
[00:40:57] Danielle: I would encourage everybody to check out our
organization, ride the omnibus. You can find us at Omnibusride.Com be
looking probably later next year. We're going to have a documentary
coming out on medical gaslighting, which is very near and dear to
everybody who has struggled to get a diagnosis or to get the proper
treatment because the doctor's not listening to you or because they're
telling you it's in your head or whatever.
I am not terribly active on social media, but I do check my email fairly
regularly, and it is 1in20000special@gmail.Com. And the reason for that
is because the odds of having both rheumatoid arthritis and primary
biliary cholangitis, which are my two primary diseases is about one in
20,000.
[00:41:43] Tiffany: Wow. All right. And you can find me, anywhere you
find AiArthritis, which is I F A I arthritis on all of the social media
channels, Facebook, TikTok, which I'm not really on TikTok, but we have
a TikTok, and Instagram, and Twitter and LinkedIn. Got 'em all up there.
You can also go to our website at aiarthritis.org.
All of the episodes are on there all of the tools we've created thus far as
people living with the diseases you'll find all kinds of resources there as
well. While there we always encourage you to hit the donation button
because we certainly can't continue to do what we do without the
support of our community And we will have on this episode page a form
so that you can share your story.
We'll also be asking for this on our social media channels. So look out
for those. Other than that, we encourage you so much to pull up the
chair, pull up a seat at this table because we cannot do these types of
solutions without your voice. Thank you all so much. Until next time.
Take care. Aiarthritis Voices 360 is produced by the International
Foundation for Autoimmune and Auto Inflammatory Arthritis. Find us on
the web at www.AiArthritis.Org Also, be sure to subscribe to this podcast
and stay up to date. Today on all the latest AiArthritis news and events..
AiArthritis Voices 360 is produced by the International Foundation for Autoimmune and Autoinflammatory Arthritis. Find us on the web at www.AiArthritis.org. Also, be sure to subscribe to this podcast and stay up to date on all the latest AiArthritis news and events.