Undifferentiated Disease - What is it & How Could a Diagnosis Affect Me?
AiArthritis Voices 360, Episode 106
Air Date: January 31, 2025
This episode is a Step 2, as outlined in our 6 Step Patient-Led Problem Solving Process.
What does it mean to be diagnosed with undifferentiated disease (UD)? In this episode, Tiffany
Westrich-Robertson, AiArthritis CEO and founder, unpacks this complex diagnosis, sharing her
personal journey from being a mystery patient to receiving a UCTD diagnosis. Tiffany explains
how undifferentiated disease fits into the autoimmune.autoinflammatory spectrum, its
implications for treatment, and why early intervention is critical.
Join us on this episode to explore what undifferentiated disease means, how early treatment
can improve outcomes, and the latest research shaping diagnosis and care.
● Tell us YOUR undifferentiated disease story: https://bit.ly/3EfuWsT
● Check out our social media channels for posts about UD and weigh in
● Sign up for our AiArthritis Research Database, where we are studying UD at www.aiarthritis.org/database
Donate to Support the Show: www.aiarthritis.org/donate
Episode Highlights:
- Learn more about undifferentiated disease, including why it’s so important to know it can be the final diagnosis OR it could branch off to a “full blown” autoimmune or autoinflammatory disease, including one of ours that include inflammatory arthritis as a major clinical component. Either way, UD IS a real diagnosis.
- Explore the connection between undiagnosed “mystery patients”, an undifferentiated diagnosis, and how UCTD and other undifferentiated conditions fit into the spectrum of autoimmune and autoinflammatory diseases.
- Understand the importance of early intervention and how it can lead to remission and improved outcomes.
- Discover the role of biomarkers, precision medicine, and risk stratification in guiding treatment plans.
- Hear how AiArthritis is advancing research and offering resources to help patients navigate undifferentiated disease.
AiArthritis Voices 360 is produced by the International Foundation for Autoimmune and Autoinflammatory Arthritis. Visit us on the web at
www.aiarthritis.org/talkshow. Find us on Twitter, Instagram, TikTok, or Facebook (@IFAiArthritis) or email us (podcast@aiarthritis.org). Be sure to check out our top-rated show on
Feedspot!
-
Expand to View the Podcast Transcript
[00:00:00] Intro: Welcome to AiArthritis Voices 360, the podcast solving today's most pressing issues in the AiArthritis community. We invite you all to the table where together we face the daily challenges of autoimmune and autoinflammatory arthritis. Join our fellow patient co hosts as they lead discussions in the patient community, as well as consult with stakeholders worldwide to solve the problems that matter most.
Whether you are a loved one, a professional working in the field, or a person diagnosed with an AiArthritis disease this podcast is for you so pull up a chair and take a seat at the table
[00:00:46] Tiffany: Hello and welcome to AiArthritis Voices 360. This is the official talk show for AiArthritis, which is short for International Foundation for Autoimmune and Autoinflammatory Arthritis. My name is Tiffany Westridge Robertson. I am the original founder of the organization, CEO, and person living with non radiographic axial spondyloarthritis, among some other conditions as well.
And this is a very special episode for me personally. Because one of the reasons I founded this organization was because I started off as a mystery patient and then quickly after that diagnosed with what's called undifferentiated connective tissue disease, which falls under the umbrella of undifferentiated disease, which we're going to talk about today.
What is this diagnosis? And how could a diagnosis like this affect me? And what does it mean in the realm of moving on to another diagnosis or staying with this diagnosis? And you know, I have to say, back in 2007, when I went from mystery patient to undifferentiated connective tissue disease, it was presented to me as if this wasn't a real diagnosis.
They, the doctor who was a rheumatologist, essentially said it's something connective tissue, which means it could be RA, it could be Sjogren's disease, it could be scleroderma, it could be lupus, it could just be many of these things. But it's too early to know is the way that it was, it was framed to me because essentially undifferentiated means the symptoms could be sort of all over the place, but none specific enough to go under a classification of a different, I'm going to say a different specific disease because that's where I got confused because it's often it'll be said it's not enough to warrant a diagnosis.
Well, it is a diagnosis. Undifferentiated disease is a diagnosis. And I'm going to talk a little bit today about why that's important for patients to understand, because it impacts not only just the mental overview of it, but also treatment plans and in prognosis. So essentially, I was told you have the, so going back to my story, I was told, okay, you have this disease, so what are we gonna do about it?
And the, and the answer that I received was, well, I need to know what this may turn into, and for that reason we're going to wait and watch you get worse. Again, this was back in 2007, and I did get worse. I got a lot worse. And I ended up getting so bad over about an eight month, eight month period that I couldn't hardly stay awake.
I was sleeping about 16 hours a day. I, because of this extreme fatigue, I felt like I, kind of had the flu all the time. I had a, I did have an array of different symptoms. I had sort of this joint pain. I had pain in my tailbone. I had pain on kind of one side of my body. It wasn't on the other side, which is very indicative of rheumatoid arthritis.
I was getting little like canker sores on my tongue, and they're like, well, I don't know what that has to do with anything that kind of goes along with Sjogren's disease a little bit. And so there was no definite arrow pointing in one direction. It was kind of like, could this be spondyloarthritis? Could this be RA?
Could this be, could this be, could this be? And it made me feel incomplete. It made me feel like, okay, they're telling me there's nothing we can do and I can't be treated. And the only thing that is a solution is to wait and get worse, which was unacceptable. And that really was my inspiration for starting this organization, which is turned into a full fledged foundation, and we're going to talk a little bit about how this, the work that we're doing with undifferentiated disease and educating you today can also lead to some of the other programs we're doing in the research department in particular.
So first of all, have you been diagnosed with undifferentiated disease or a variation of them? This could be undifferentiated spondyloarthritis. Sometimes you might hear an undifferentiated autoinflammatory disease or an undifferentiated autoimmune disease. It's a kind of unfortunate there's so many that could fall under this umbrella.
The most common you'll hear is undifferentiated connective tissue disease though. And, while there is no specific Diagnostic criteria, even today, which blows my mind for undifferentiated connective tissue disease, it's more further along in research and an understanding of what it is than some of the others that I mentioned.
And so I think for that reason, it's often the go to of the things that fall under the undifferentiated disease umbrella. So. First, I'd really love to know, have you been undifferent diagnosed with any of the forms of undifferentiated disease? And please tell us, we're going to be posting this on social media and we also will have a blog post about it on our website.
And we would love to hear your story because we have a very strong focus on this because we have always believed since our inception in 2011 based on listening to patient voices and patient stories like my own that most of us start at some where we could possibly get this diagnosis of undifferentiated something, connective tissue disease in my, in my case.
But what mostly happens is patients will often have many of these symptoms and they get no diagnosis, so they're just, stay as a mystery patient, but it could be a diagnosis. And why is that important? Well, studies show anywhere from like 15 to maybe 30 now, they've gone up a little bit, are patients that actually have an undifferentiated disease.
AiArthritis believes it's more like 50%. And we proved that theory in 2013 in our first research project called the Early Symptoms of AiArthritis diseases and we will link to this project for you. It's very fascinating. We there was hundreds of patients around the world who participated and while approximately 15 percent which is in keeping with publications were in fact diagnosed with undifferentiated disease first.
Another 37, 38 percent met a kind of a criteria of what could be diagnosed as undifferentiated connective tissue disease, meaning they had the fatigue, they had random joint pain and some of these other rashes or other symptoms that fall under that, but they had no diagnosis, or if they did, they weren't told and it lead and it was 54%. So we consider this a high priority diagnosis for that reason. Secondly, because we want patients to be proactive about getting on a treatment plan if they are diagnosed with this undifferentiated disease. Why? Because we already know that early intervention is the best way to achieve remission. We don't often hear remission in our diseases, and that's Too often because of a delay in diagnosis, a delay in treatment patients feeling like maybe I'll, I'll wait and watch till I get worse and before I start a treatment, but research after research after research shows early intervention has better outcomes because you actually can go into remission and maybe never have to be on medications for the rest of your life. It's possible, but it's possible most often with early intervention and there's no earlier than undifferentiated disease. So there's a lot of studies. We do a program called Go With Us to conferences, primarily the American College of Rheumatology every November.
And also EULAR, which is the European Congress, the European Rheumatology Group. And that happens in June. So make sure you sign up for that. And part of that is we go to these sessions and we learn about what's happening in research, what's happening in our diseases, in our treatments. And one of the focuses that I have seen over the last few years is on differentiated disease.
So at EULAR 2023, I went to a session and we will link to a clip. There's a clip on YouTube. You can hear me talking about this. And we're also, as I mentioned, going to have a blog post and doing a lot more work in, in undifferentiated over the next several years. So we, you definitely listen to that, but it started talking about how researchers and doctors are really focusing in on this as an early disease.
And that is important because they're starting to also sort of create this line of when are you undifferentiated disease, and you might stay undifferentiated disease, which I want to say again isn't a bad thing. I thought that was a bad thing is not a bad thing. It just simply as long as you get treatment that I think that's the important thing here and you don't wait and get worse.
So treatment intervention when there's undifferentiated disease, important, important and contact us about how to talk to doctors about that. That's one of the things we want to pull out of this episode is creating. Patient peer led recommendations working with our rheumatologist to to create a dialogue on how if you have undifferentiated disease, you can talk about interventions and treatments.
So what the research is showing is there's this break where they're starting to identify, in some cases, based on biomarkers, which are, they'll take your blood, they'll look at different markers, like you may have heard of rheumatoid factor, or ANCA, or just different biomarkers, different readings in your blood that may Indicate this could be a going closer to sjrogens.
This could be going closer to lupus that paired with certain symptoms. So take lupus, for example, certain biomarkers may point to it and then you may have a molar rash of rash on your face. Then they start to start looking down. So there is efforts to start to kind of rearrange the symptoms and say, symptoms plus biomarkers and undifferentiated could lead us down this direction.
And maybe that's a better way to think about early intervention and treatments because even though many of our diseases are treated with the same biologics, there are different biologics that work better for different diseases. So there's going to be some that are going to work better for lupus than rheumatoid arthritis, for example.
And that's one of the reasons that this kind of early treatment of undifferentiated disease is, is up in the air because the doctors don't want to put you on the wrong direction. In saying that, what are current treatments? So often, they will start you on an NSAID, so think of like an ibuprofen maybe prescription level, maybe not, and that's what I was started on, because I, I had also this terrible pain in my chest, which is called costochondritis, and what I learned later in my education of going to these conferences and the program go with us to conferences is that that is a form of what's called enthesitis, and that is an inflammation and the kind of where the tendons and the bone connect in your ribs.
So it almost feels like a heart attack. And so that was one of my undifferentiated signs. But enthesitis, is very prominent in spondyloarthritis diseases, which is my current diagnosis. So if you kind of think about this, Ooh, let's track my symptoms. I have undifferentiated, let's work with the doctor.
Maybe if I get some biomarkers that point in a direction, maybe if I pick and choose these symptoms, it can start a map and it can get them to some better answers. But in the interim talking about what can we do for intervention? Is it at least some kind of NSAID, right? Then there's also discussion of starting on a demart or disease modifying agent, which could be like a methotrexate.
There's a common, um, I'm on leflutamide, for example. So there are the, that's kind of like the next step. There are some patients who hydrochloroquine and, or hydroxychloroquine, excuse me. And that is often if you're more on, it's seeming like a lupus route and steroids. Now, there's a lot of movement to, to move away from the steroids, very short term type of situation because we need to get patients off of long term steroids.
So that's another reason why kind of talking about the options and maybe an earlier, more aggressive intervention could put you in remission. So those are the things we're trying to study and work on at AiArthritis. And saying that, so that's what undifferentiated disease is, and sort of how this diagnostic or kind of figuring out this mystery goes, and also that it is a real diagnosis.
So I want people to feel like they, like, They have some kind of answer because I know when I had it I just felt incomplete and I don't want anyone to feel that way. It is a real disease and it may never progress to another disease and that's okay. Often that means that the outcomes aren't as severe. So don't look at that as a negative.
Look at it as a last half full, right? The outcomes usually don't lead to the joint deformities or such aggressive comorbidities or additional diagnosis. So if it doesn't get to the point where this looks like it's breaking off and it's staying in undifferentiated, that's not a bad thing. The other thing that we wanted to talk in this, so we talked about what it is and how it, how kind of how the diagnosis could affect you, and then kind of what are the next steps.
We talked a little bit about treatment. What can you do? You're diagnosed with an undifferentiated disease. What happens next? Well, as I mentioned, there's a few things that we would like to help as peers help you when you are diagnosed with this disease. And the first thing is let us know your story.
Even if you have progressed from undifferentiated like me, we still want to hear your story because we are starting to do research specifically on this disease to help researchers and doctors with this disease with identifying it, identifying more where that break is, where it might progress to a different disease.
Dialogue about treatment and disease management. We really want to be at the forefront of this, and so in doing that we want to hear from you. That's how all of the data that we collect starts. We listen to our peers and we start to figure out what you need. And that's the first step. So make sure you click on the link to this episode and fill out the form to tell us your undifferentiated disease diagnosis story.
Secondly, we want to make sure that you are understanding the potential treatment plans. So we want to make sure that we give you guidance and you can contribute to helping us create this guidance as we navigate through undifferentiated disease to make sure that there is a treatment plan and wait and watch it get worse.
We want to really politely push back on that or at least get more context to this because we know that it's something that we don't want to push off for too long. Start thinking about when is the break off point where, where it starts to become another, another disease and then we even with that, that becomes an early intervention for a lupus or an early intervention for a psoriatic arthritis, early intervention for a Sjogren's.
Let us walk you through that path. The third part of it is how you can get involved past sharing a story and past participating in these kind of guidance and diagnostic guidance and communication with our doctor guidance that we're working on. The third part is research AiArthritis has launched the Aiarthritis Research Data Bank, which is living inside Forward National Data Bank for Rheumatic Diseases. It is an international data bank and it is designed for our two dozen diseases. One of the focus features that we're doing is we're studying undifferentiated disease and the mystery patient. So, since we know because of the study I referenced earlier with the early symptoms of AiArthritis diseases that we led in 2013, we know that about 50 percent of patients will meet some type of criteria that falls under this undifferentiated disease, even if 15-30% percent of them only have the diagnosis.
So if you have certain symptoms, and we will list the symptoms that you're going to fall under could be a variety of pick and choose can be fatigue is almost always involved some level of kind of joint pain, then it can branch off to. Your eyes are infected your certain organs may infected. I mentioned canker sores.
You could have rashes. You could have different levels of muscle pain. There's it's like every symptom that could be associated with any of our diseases could fall under it and that's what makes it so confusing, but if we get you a checklist and help you to start navigating this and then also invite anyone who doesn't even have a diagnosis yet, but meets all of this kind of criteria.
So maybe you do have it. We want you in the database because the goal is not only to follow people through a diagnosis with our help on the side, so it's not even just a regular database or research, you would be working with your peers to get some guidance and get some health education along the way.
And tips on how to speak to the doctors to navigate through this. So we're there for you in addition to the research you're getting in addition to the research, you're getting guidance along with it. So then our goal of that research is to identify people in real time, getting the diagnosis. How long did it take?
Why? We can go back and start asking you questions. You can be part of conversations. We as patients start to figure out the why, why did this take so long? And then we can work with the researchers to try to find novel ways of identifying these diseases earlier, better ways of talking to the doctors to expedite diagnosis.
And then also those with existing undifferentiated disease, we really want to study how many are moving on to other diseases and where is that breaking point that we're starting to see at these conferences where they're starting to look at what the breaking point looks like we want to help these researchers by capturing that.
So I really hope that you will participate in our work. To help those diagnosed with undifferentiated disease and also to help with our research and education, health education work to help those navigate those with this diagnosis or mystery patients navigate through getting to either staying at an undifferentiated disease diagnosis or moving on to the next, helping research, advance our treatments, We can do this together.
So, thank you so much for tuning in. We know there's a lot of you out there. We understand. We say we don't represent the patient voice. We are the patient voice, and we stand true to that. So, thank you for joining in on this episode of AiArthritis Voices 360. I'm very excited to be personally working with many of you around the world on this very important initiative.
Also, when you're checking out the episode on our website. Check out all of them. We have over a hundred. What? It's true. And also hit that donate button because your gift helps us be able to continue not only the show but all of the work that I just mentioned in research and health education being able to have peer to peer conversations and support.
We do a lot for our community thanks to your support. So thank you for that. Alright, that's it. I am signing off here from AiArthritis Voices 360. Have a fabulous day and don't forget to pull up your seat at the table. Because only when we unite. Can we make change?
[00:21:44] Intro: AiArthritis Voices 360 is produced by the International Foundation for Autoimmune and Auto Inflammatory Arthritis.
Find us on the web at www. aiarthritis. org. Also, be sure to subscribe to this podcast and stay up to date on all the latest AiArthritis news and events.
Intro: [00:00:00] Welcome to AiArthritis Voices 360, the podcast solving today's most pressing issues in the AiArthritis community. We invite you all to the table where together we face the daily challenges of autoimmune and autoinflammatory arthritis. Join our fellow patient co hosts as they lead discussions in the patient community, as well as consult with stakeholders worldwide.
To solve the problems that matter most, whether you are a loved one, a professional working in the field, or a person diagnosed with an AiArthritis disease, this podcast is for you. So pull up a chair and take a seat at the table. Hey
Leila: everybody, and welcome to AiArthritis Voices 360. This is the official talk show for the International Foundation for Autoimmune and Autoinflammatory Arthritis, or AiArthritis for short.
My name [00:01:00] is Leila P. L. Valete and I am a person living with lupus and Sjogren's disease and the health education manager here at AiArthritis. Today is a special episode to report back on breaking research in the rheumatology community. Me and several members of our team were in Washington, D. C. this past week attending the American College of Rheumatology or ACR Convergence.
We attended several sessions and reported back on topics that we felt were important for patients to learn about. So please enjoy these four research updates.
Tiffany: Hi everyone, this is Tiffany Westrich Robertson reporting to you live from the American College of Rheumatology. Conference 2024, and I am a person living with non radiographic axial spondyloarthritis.
On this segment of the debrief, I'm going to focus on new therapies for our diseases, which are focusing primarily right now in lupus, but [00:02:00] also in some diseases like myositis, and systemic sclerosis as well or scleroderma. But in this particular model and the one I'm going to talk about today, they are both in lupus.
And so if you're asking, why do they always start in lupus? Lupus is a very complex disease, one of the most, if not the most, in our group of a couple dozen diseases. And so if they test in one of the most complex ones to begin with, it's easier to adapt as they start to move into other diseases. So don't be discouraged if you're like, why is it lupus?
It's, that's the reason why. So I'm going to cover two different types of cell therapies. That's the big hot topic at this ACR 2024. And this is a, these are different. than our current biologics. These are using our own cells or donated cells in some case from others depending you're going to hear about both of those situations today in [00:03:00] my report and then infused back in the body to deplete other cells and in a, and they don't know the exact reason why it works, but it ends up putting most people into remission, in complete remission.
So very different than the biologics where we might do a trial and error and then we might have some improvement but we still could flare, that type of thing. So these are very, cutting edge type of therapies early in the process but exciting all the same. So the first one that I'm going to briefly talk about was presented by Bristol Myers Squibb, or BMS, and this one is specific to CAR T, C A R dash T, and essentially in these studies for lupus, they take your T cells, they draw them from your body, And then they go to a lab
[00:04:00] and they essentially modify these T cells and they will infuse them back into your body.
So it takes about two weeks before the re infusion happens and in the interim, they do a mild form of chemotherapy to then deplete your B cells so that as this gets infused back into your body, there's no type of reaction, everything is starting fresh, and it is a reset. That's a big word I kept hearing all through ACR2 was a reset because of this new cell therapy.
So once these patients have been treated, They are coming back with little to no disease activity, primarily a hundred percent remission. They talk, they had some people from the cancer community there because this started in cancer, now it's moving to autoimmune. And the cancer patients who had lymphoma and went through this all are in complete remission seven [00:05:00] years later.
And they said, The C word used to stand for cancer, now it stands for cure. That's a word that we are also not familiar with in our communities. The fact that these types of therapies are on the horizon is super hopeful. The second one, Deb and I met with a company called Arteva. And they are also working in cell therapy, and this one's just a little bit different.
Focus also on lupus with or without nephritis, which means the kidney involvement. And their CAR T therapy is not pulled from your two T cells from your body, instead it is donated through the. It's, they said borrowed cells from donated umbilical cord blood. And so these therapies then are infused back into the body.
And in this case, there is not that you don't have the mild [00:06:00] chemotherapy part in it. So that part is removed. There's also not a hospitalization part of it. So this is more considered an outpatient type of situation. It is a deep B cell depletion. And the fact that they keep kept stressing the outpatient administration and only if there were any potential side effects, complex patient would anyone be in hospitalized for observation.
So this one is just another option that is being tested. There are current clinical trials on this and we're getting more information about those. And cool. This is an exciting time for our diseases. I, Deb and I were talking earlier and thought, man, in 10, 15 years, it just might be like the new treatment, the new wave of the future.
The biggest obstacles, obviously affordability. So we don't, these are going to be very expensive. We do not know how government healthcare systems, [00:07:00] how we will gain access to those. But we know that the if there's a one time situation where you go into remission and you don't have to actually take these expensive other drugs all year round, that is a huge savings.
But the other issue is we don't know how long these last. So we can say that like in the people who received these CAR T therapies five years ago, three years ago, seven years ago. They're all still in remission, but we just don't know how long it's going to last. And so that's still to be determined. And that's going to really weigh heavily on how do you cost this out when we don't know if it's one time or two times in a lifetime or 10 times in a lifetime.
So still a lot of research that has to be done in that respect, but really exciting times for all of us. So there you go. There is my update on cell therapy.
Leila: Hi everybody, this is Laila, [00:08:00] Health Education Manager here at AiArthritis, and I am here to debrief day two of ACR 2024, or Sunday. So yesterday was Sunday. I'm recording this Monday morning because yesterday I had a bad day. I was very tired. And so I ended up going to one session, but I also ended up being able to read some abstracts and go to some of the abstract sessions.
The abstract sessions are a long session in person, they're about an hour and a half. And they have little 15 minute segments of different abstracts that are under each different category that they have. So I was able to attend. Some of the weight loss, some of them that had a weight loss in it, as well as information about pain.
Okay, let me correct myself. It's not about weight loss, it's actually about obesity and how obesity can affect inflammation. And the prevalence of obesity [00:09:00] in autoimmune diseases, is, it's pretty significant. So in RA, they say about 14%. Patients are obese in lupus, it's about 14%. And in psoriatic arthritis, it's about 20%.
And so in psoriatic arthritis, They exhibit higher odds of developing, so obese individuals are more likely to develop psoriatic arthritis. And so that was a very interesting thing to learn. I had never heard anything like that before in terms of how likely you are to develop an autoimmune disease if you are obese.
And I have been obese my whole life. I actually had weight loss surgery last year, the vertical sleeve gastrectomy, in order to help with my obesity. And even though I got weight loss surgery and did lose a good amount of weight, I'm still considered [00:10:00] obese and I will still be considered obese probably my whole life because of my BMI.
And so it's very interesting to learn how obesity can affect these autoimmune diseases. And from this abstract, that's really what I learned was the prevalence of obesity in the autoimmune diseases that they studied. And they do have recommendations and actionable tips in order to help with obesity.
Discussing your weight with your providers, incorporating a balanced diet and exercise, things that we all know about and do try to incorporate in our lifestyle. Although it doesn't account for, the recommendations that they give don't account for the symptoms that we may be experiencing and that may prevent us from, you know, exercising on a daily basis.
Or as much as we'd like to, or the motivation for us to be able to [00:11:00] exercise and be able to cook for ourselves healthy food and things like that. Yeah, hopefully, because they know this now, that these patients are more likely to have these autoimmune diseases and have obesity. Then maybe there will be a next step afterwards on tailoring specific programs for obesity for those who have autoimmune disease.
For me, my autoimmune disease or my lupus was not considered in any of my weight loss programs. I don't know. technically look like a unsuccessful weight loss surgery can't patient because of the outcomes that came from my surgery. It wasn't enough of my body weight to be considered successful in the amount of time that they deem.
But also what we need to know is that In order for your body to lose weight, you have to be healthy in order to be able to [00:12:00] lose the weight, your body has to feel like it's in an equilibrium and homeostasis of being at a good place, like not your immune system is not super overactive and there's not infections going on and things like that because it's just not the In the beginning, after I got my weight loss surgery, I had a bunch of UTIs.
And those UTIs, I felt, kept me from losing as much weight as I should have in the beginning because my body just was freaking out. I just had this surgery and I'm having an infection. It's trying to, you know, balance out and figure out what's wrong before it is allowing you to shed the weight. And so that's just one thing is that.
In order to even be able to change anything about weight, appearance, anything like that, you have to be healthier overall in order to even have your body allow you to do that. So of course, no matter what, even if it's not to lose weight, exercise is [00:13:00] always so good to help with the joints, to help with movement and just overall wellness.
But in order to really lose weight and lose weight hardcore, you have to be healthy. And so I just want to say that with obesity and with weight loss and how much in America we do try to push weight loss and there's a lot of that conversation going on now. Just remember that your body is fighting its own fight and it's a lot, it can be a lot harder for us to lose the weight.
So I just wanted to make sure to give that validation to everybody because I know that weight is something. that a lot of people with our conditions struggle with. Another one of the abstracts that I went to was about chronic pain. And it was about pain disability reduction. So participants who partook in the, who completed this study, they reported a significant decrease in pain related disability.
[00:14:00] And that's amazing. Pain can debilitate a lot of us in a lot of ways. And so this was mainly for older adults. And they practiced self management, a self management program and provided tools and strategies to help manage chronic pain. The program, it offered varying benefits on individual factors such as age and socio economic status.
So they helped. They tried to do their best to meet the patients where they were and what they could accommodate for. And so I actually pulled up the, so this program is from Stanford and it's called the Chronic Pain Self Management Program. And these are the different tips that they have developed after going through this program with this first set of cohort.
And these are the tips. One, determine how you spend your time. Keep a diary of how long it takes you to do activities and how long you need to rest for in order to recover. [00:15:00] Two, make a schedule. Develop an activity schedule that includes rest breaks and stick to your schedule. Three, be time oriented, not pain oriented.
Knowing how long you can do an activity before your pain gets worse means you can schedule specific activities for a certain number of minutes before taking rest for a specified period of time. And this keeps you not in pain, but in control. Rest before your pain starts to get worse. Because so many times we want to complete activities and push through pain to keep schedule, but stop and make sure to take a rest.
I needed to learn that yesterday when I was not feeling well after pushing myself so hard the past week. to prepare for the conference. 5. Incorporate change into your activity routine. A change may be just as good as rest. If you're in a situation where you can't take a rest break, alternative activities frequently, changing body position, stretching, or going for a walk.
Use a [00:16:00] timer to signal breaks. I actually, me and Deb were just talking to Tiffany about this morning and that we try to set timers for activities that we're doing. So in case one, we need to keep time or two, if you know that you can only do that activity for a certain amount of time before you lose focus or before you start to be in pain, that's really important to keep it, keep yourself going.
Seven, break tasks into smaller, more manageable pieces. Eight, avoid rushing, slow down, plan ahead, and because rushing can increase your stress, which therefore can increase inflammation and pain. So it's a really unfortunate phenomenon and conundrum that happens. Nine, don't overschedule activities, work on developing realistic expectations for yourself.
I still really have to work on that. I always can think that I can do more than I can. And so I end up under delivering of what I would wish I [00:17:00] could. So I need to make more realistic expectations for myself and prioritize your activities. Some days may not, you may not be able to get to everything, determine the most important thing you want to accomplish in that day, and then work on that.
And yeah, I think that those are some amazing tips. to be able to go by, and this is what the chronic pain self management program was based off of that they presented in this abstract. And let me actually read the titles of these abstracts so that if you wanted to look back, you could. The chronic pain is called impact of the Stanford University chronic pain self management education program.
on pain severity, pain self efficacy, and pain disability in a population with a high prevalence of arthritis. Speaking of older individuals. And let's see, okay, and then the other one that I spoke of is obesity and the risk of [00:18:00] autoimmune diseases. Insights from the National Inpatient Sample. So those are the two abstracts that I wanted to report back on because I thought would be very interesting to our patient population that is watching this.
And lastly, I did go to a lupus nephritis care session. It was called tester knowledge. So basically the whole session was very interesting. It was going through a case study of the patient that the researcher was studying. had in real life. And so there's, it was like a spectrum of time and different decisions that were being made in this patient's life and how the treatment that they were receiving was tailored to those different decisions that were being made during that time of life during diagnosis.
Again, it's a spectrum of the patient journey. During diagnosis, your decision making on treatment can be totally different than maybe three, four, five years down the [00:19:00] line. And basically they went through the different times when they took, different times when they took kidney biopsies to really see how bad the lupus nephritis was in that moment.
They talked about the different treatment options that there could be and that there's, no wrong answer in what they provided, but just showing that there's a variance in how every single individual rheumatologist would treat specific cases in general. And so there's always going to be different combinations of medications that they think may work well together and things like that.
So it was really cool to see how the different rheumatologists in the room would think because they were asking to raise your hand for which different treatment option you would go with. And the researcher basically said that a strategy on getting very detailed insight on what's actually going on in the body is doing a kidney [00:20:00] biopsy.
And although kidney biopsies can be very invasive, they are the only way to really know how someone's lupus nephritis is going and in what stage it's in. And she does recommend to do them often or whenever treatment changes are being discussed. And so that was a very interesting session to go to just to see how all the different rheumatologists differ in their options that they would pick and also comparing the options that were up there to the decisions that, the shared decisions that I've made with my providers, especially around family planning, on preference, whether you like injections or infusions or pills or the amount of pills. things like that. It's really amazing to see that there are a lot of different options for the medications out there and the different combinations that you can do. I also saw some information about other sessions that talked about the alternatives to kidney biopsies and so I do want to report back on that and a little bit more about some of the lupus abstracts and I will do that for my video for today.
And so thank you so much for watching. This is day two of Go With Us to ACR 2024. Today is going to be our last day of actually going to the conference. So today, Monday, and I'm excited to report back and give you my feedback from whatever happens today. I have to go and get ready now, but thank you so much for listening to my debrief.
And if you have any questions, feel free to email us back about any of these debriefs that we have. You can tag us on social media, message us on social media if you have any questions, or if you are in our Slack elevated experience, you have access to us right there already.
Cristina: Talk to you all later. Bye.
Hello, everyone. My name is Cristina Montoya. I'm a dietitian and a person living with Sjogren's disease and rheumatoid [00:22:00] arthritis. Today, I'm wearing my patient's hat to share with you a few highlights from the session I attended on day two on the novel imaging and therapeutics in Sjogren's syndrome.
This is part of the Go With Us to Conferences program led by AiArthritis, short for International Foundation Autoimmune and Auto Inflammatory Arthritis. So let's start with Dr. Alan Byrne. Dr. Baer is the director of the Jerome L. Green Sjogren's Disease Center at John Hopkins University School of Medicine.
He presented on the challenges for disease, modifying therapy in Sjogren's disease. So I just wanted to clarify that you might see the name Sjogren's syndrome, but remember that Sjogren's, the name was just changed, officially changed this year. Dr. Baer. When these sessions were submitted in 2023, it was still [00:23:00] considered Sjöbren's syndrome, so please don't get upset.
Now, this session's objective was to understand the fundamental tension between Sjöbren's disease modification and symptom relief in Sjöbren's clinical trial designs. Dr. Baer shared, he shared how Sjogren's disease has high morbidity and a high burden to the patient that included not only the sickest symptoms of dry eyes, nose, mouth, and skin and every, everywhere else, but also fatigue, morning stiffness, trouble sleeping, muscle and joint pain and brain fog.
He highlighted what patients want from us. New systematic, systemic treatment. Patients want a better management of day to day symptoms, like fatigue, muscle, joint pain, dryness, neuropathy, and dysautonomia. Patients want to reduce Sjogren's flare ups. [00:24:00] They want to reduce the risk of long term concerns by extreme dryness or lymphoma.
And stop medications like Pregnizone and other chronic medications. But what are the challenges on developing medications that can modify the disease? The main problem is that there is a poor correlation between the disease activity, which is measured by the SDA, or what is short for Uler Sjogren Syndrome Disease Activity Index, and the Symptom Burden Index that is measured by the ESPRI, which is the Uler Sjogren Syndrome Patient Reported Index.
There's also challenges in a monitored desolvary in gland dysfunction when it's already too advanced when the patient is diagnosed and it may not be reversible. And another challenge will be that the disease progression is very slow compared to [00:25:00] other rheumatic diseases. So that poses a challenge when we, when they're doing clinical trials, because they, maybe the time is just not enough to see the positive side effects.
Dr. Baker also stated that, unfortunately, the scores used to measure the disease activity do not fully capture the disease systemic involvement. According to the S day, 15% of patients will develop severe systemic disease, but up to 50% of patients can develop systemic manifestations in other autoimmune diseases over 10 to 20 years.
You see, it's like varies and that also interferes with early diagnosis and detection of the disease. The current limitation of clinical trials is that they target select populations. They do not include seronegative patients, or at least not for now, and they identify that there is a robust [00:26:00] placebo effect.
So they need to decipher whether it's the effect from the medication or it's the placebo effect. In some studies, although there is a statistically significant response, it is not always reflected on how the patients feel, meaning that the biologic effects do not translate into the clinical effects. He said that it's possible that patients need that extra time to, in those trials, for the effect to be seen.
Better better outcomes could be obtained if there were better tools to exclude the non autoimmune Zika, if there were tools to predict the evolution of Sjogren's with those with Zika and or anti SSA positivity, and a better understanding of the symptom etiology. As a patient, I felt validated by Dr.
Baer because he explained the barriers and limitations And he also shared what are the patient's [00:27:00] expectations from these clinical trials. So I truly appreciated this session. The next one was on the novel imaging to diagnosis Sjogren's syndrome, cutting edge techniques. So this one was by Dr. Josevar from Slovenia.
And just like I said on the title, it says Sjogren's syndrome, but then she's right from the get go. She said, I'm going. To talk about Sjogren's disease. So that was very validating as well. This one was a little bit over my head because there was a lot, they were just basically talking about advancing the, and utilizing the ultrasound of salivary glands to diagnose and potentially evaluate the progression of the disease.
Because she indicated that to this date. We don't have a hundred percent sensitivity diagnostic test or diagnostic [00:28:00] criteria for Chagrans, which delays the diagnosis and treatment. As we all know, the technical, basically the doctors utilize the classification criteria, which is not the same as a diagnosis criteria because technically it doesn't exist yet.
So it takes a full expert. like clinician's expertise to, to see the patients holistically beyond the Zika symptoms. The, so again, so then she explained that using the ultrasound of the salivary glands and also MRI. in xylendoscopy, so basically it's just an endoscopy that goes directly into the salivary gland.
Could potentially determine or detect the Sjöbren's disease a little bit earlier, but despite these potential imaging techniques for diagnosing Sjöbren's, to make the Sjöbren's diagnosis possible. There must be a comprehensive [00:29:00] clinical histological imaging test to confirm the diagnosis and not just to rely on the testing of the salivary glands, especially when the results are not conclusive.
Remember that a lot of patients, because the disease progresses so slowly, they do not die. Thank you. present the histological changes in the salivary glands. Unfortunately, as a patient, I saw that the new testing, again, is very focused on the salivary glands and not on the systemic involvement of the disease.
And the last session was presented by Dr. George Booyen from the Netherlands. And it's quite funny, but it's also very interesting because he walked us through all the clinical trials that had been conducted on chauvrins for the past 20 years, I will say. And my, what I could determine is basically all of them had [00:30:00] failed.
That they moving to like phase two, and then when basically says there's no significant changes on symptom burden or biological changes, there was someone in the audience with Dr. Bookman, he is our show brands expert in Canada. And he asked, and they specifically say, maybe we're just not giving enough time to these trials and enough time to the patients to feel the real effects.
They also talked about that perhaps we are still identifying part of the immune cells that they need to target in children. So currently there are over 20 clinical trials on patients with Sjogren's, which is really revolutionary and is very new. Three are currently in phase three, meaning that now they're expanding the results to a larger population.
The good news is that pharmaceutical companies prioritize drugs. for autoimmune diseases. This means [00:31:00] that, but it's still, we need to be like cautiously optimistic, really indicated, let's not promise anything to the patients yet. We have to see the results of these clinical trials. My takeaway from this session is that at least one clinical trial is showing some early positive results and moving to phase three.
And, but overall there's been, I saw more abstracts inside scientific sessions on show brands. than any other years. And I couldn't even enter one of the sessions on Saturday because there was an overflow of people wanting to learn more about Sjogren's. So I can see the light when it comes to Sjogren's disease.
So I hope this was helpful for you and I'll give you another update tonight or tomorrow. Bye. Hi there, everybody.
Deb: Today is the end of day two and we've seen lots and lots of stuff. You can see we're back at our Airbnb and I'm already in comfy [00:32:00] clothes. I'm wearing red because of AiArthritis colors. So I just wanted to kind of preface that for everybody.
The debrief I'm doing today is specifically on menopause and rheumatic diseases. So you're going to see me looking over to the left here, my left, I don't know what's going to look like for you guys, but my computer sitting over here with slides that I wanted to specifically talk about. So you can take a peek and just again, apologize for my eye contact being over there.
But it's the best way so you guys could hear everything that I learned today. So today, the first part of the menopause section had two parts. So the first one was transitioning through menopause, implications for patients with RMDs, and the speaker was Sharon Parrish. She's from Weill Cornell Medical College.
Not sure where that is, but she [00:33:00] did a fabulous job. The learning objectives of this particular piece was recognizing common perimenopause and menopause symptoms in patients with rheumatic diseases and including those which that have a little bit of a differential. So they also have, they speak more about the flares that we have and things like that.
And also talking about the psychological changes. that we all have during that time, because there are many. I've been through it, so I know. Then we move on to the symptoms of menopause. The typical things that we always talk about are changes in our menstrual cycle. There's the hot flashes, sleep problems, mood dis big mood disturbances, and depression that can go with it.
Vaginal health. [00:34:00] and sexual, sexuality that can have some issues, bladder control and infections leading to more incontinence and things like that, weight gain, and joint pain, of course. One thing she's focused in on are called vasomotor symptoms, S, and it affects 50. to 82 percent of women at some point during their menopause transition, and it talked about ethnic and racial differences in the black, Hispanic, white, Chinese, and Japanese women.
When it talked about hot flashes, what occurred during the day, There's the night sweats, which happen at night, common sense as far as that goes. And it talked about sometimes you can even be sweating so much that all of a sudden you get the chills [00:35:00] because air is hitting you and you're soaking wet, is your hair's wet and things like that.
So you can actually even get chills that are associated with that. Heart palpitations and let's see, just different things. So it talked about also the menopausal cysts, excuse me, I'm tired, symptoms and the burden of those other symptoms. So the primary ones that we talked about were the primary one that was number one issue was sleep.
Next one was self care, next one was work, and the next one was your mood and your emotions being all over the place. And they also talked about hot flashes being another one of the number one symptoms that had a huge burden on folks. premature menopause. So that is talking about [00:36:00] they, they actually did a study that talked about the primary ovarian insufficiency before the age of 40.
So that's very young for menopause to actually start forever. And it talked about just all the different things that can happen with that with adverse long term health consequences, coronary heart disease, osteoporosis, mood disorders, and elevated risk of genital urinary system. All of the urinary tract infections that we can get as well as dryness and things like that.
So that was definitely talked about and just, it made it feel, it made me feel better because again, I've been through so much of this that I wish I would have known this information ahead of time. Let's see, they talked about [00:37:00] risk factors for some, a lot of these symptoms that we were talking about, obesity, smoking, low socioeconomic position, high fat and high sugar diets.
None of the things we want to talk about, right? Medical comorbidities, et cetera. So menopause and. They talked about the mean age that menopause tends to happen is 46 years. So roughly into your 46th birthday. And they said early it happens there tends to be a little bit more of a risk of early menopause in lupus patients. There was, let's see, they also said that after menopause that your symptoms for lupus may improve. So that's a highlight. So again, nobody wants to go through [00:38:00] this, but we all have to pick and choose what we're looking forward to. Let's see, menopause and rheumatoid arthritis. They do say that there tends to be a lot of inconclusive data.
So They're not exactly sure at this point as far as the effect on and the severity and onset. They also mentioned that there's not a lot of studies on menopause. And definitely when I was going through it, my symptoms increased and were exacerbated significantly. Not that's going to happen to everybody, but That's my own experience, and I'm only 55.
Let's see, extreme excess bone loss is seen in RA, and increased osteoporosis that they talked about. Managing the symptoms, so it's funny, They talked about addressing the hot flashes with hormone and lifestyle interventions, diet, exercise, supplements. It [00:39:00] depends on if it's counterintuitive for you to actually go on to estrogen.
They talked about sleep disturbances and all of those kind of things. And also just really the sexual function. So having sex gets more difficult. So there are things you can actually do. which I'll get into, that can actually help your symptoms. Comprehensive care post, so after menopause is finished, is lifestyle organization, dealing with your nutrition, taking a good look, physical exercising, reducing alcohol consumption, and not smoking.
There are some non hormonal therapies to deal with some of these symptoms and they talked about a, I might say this wrong, paroxetine, which is [00:40:00] a low dose. There's mesylate salt, which is FDA approved. There's a Kynan B antagonist, which also is FDA approved and should help with symptoms. Other off label things are like serotonin and gabapentin, which some of you might have heard of.
And as far as dealing with some of the issues with the urogenital areas using moisturizers, lubricant, and be alert as far as if you're not having sex quite so often, then you might want to lean more on these type of things. They talked about using actual lidocaine in your vagina, so it doesn't hurt so bad because of the other things that we were talking about.
Look into actual different positions, so it actually is more comfortable for [00:41:00] the woman. And also talking about counseling for things like talking to counseling about your fatigue and things that really are bothering you and having really good communication with your doctor. The key points, again, is some of the things I talked about, all the different indications and the pain, sleep disorders.
Difficulties and things like that for lupus patients, they may be influenced by your menopause status. So whether you're feeling better or not feeling so good, there's definite things that lead to that. The osteoporosis in menopause. rheumatic diseases and bone fragility. So definitely keep an eye on all of those things.
Second section was related to menopause treatment options and safety considerations. And it was a doctor from [00:42:00] Weill Cornell Medicine. And she talked a lot about the risk assessment. of cardiovascular disease and breast cancer. So depending on your breast health and cancer status, if there's anything going on, it, they definitely have done some studies leading to just looking into women that are at risk for cardiovascular disease or breast cancer.
And it was definitely conclusive that you just need to follow what your doctor's telling you. Let's see. There was a piece that was done on 351 menopausal patients that either had inactive disease or active disease and it talked about this is for lupus patients and Looking into the [00:43:00] symptoms and using estrogen versus a medication and it definitely showed that the group with the hormone therapy did better.
So if you're able to take hormones, that actually helped in this situation. This one. And this last study was specific to short term hormone therapy. And it definitely was associated with helping decrease the flares in people with the rheumatic diseases, and this is specific to lupus and RA. Those are the things and some of the takeaways I had.
Again, I've been through most of this, so I totally understand that it is a really significant problem. topic for us. And again, me being 55, I had a hysterectomy, had my [00:44:00] ovaries left, then had one ovary taken out. And because it was very cystic and it was problematic. So then after that I went into horrible hot flashes at least 20 a day that were like hair soaking, clothes soaking, and I had to change my clothes at least five times a day.
So not a fun period to go through, but with hormone therapy for myself, it has actually worked, helped significantly and really held off a lot of the other symptoms that they were talking about. So definitely happy to be here and ask questions if you haven't.
Leila: Thank you for joining us today for episode 104 of AiArthritis Voices 360 Talk Show.
If you are interested in learning more about our Go With Us to Conferences program or watching our content from previous scientific conferences, you can visit [00:45:00] www. aiarthritis. org slash conferences. And if you love programs like our talk show and Go With Us, Please show your support at www. airarthritis.
org slash donate. These programs are only able to keep running with your support. Thank you all.
Intro: AiArthritis Voices 360 is produced by the International Foundation for Health. for autoimmune and autoinflammatory arthritis. Find us on the web at www. airthritis. org. Also, be sure to subscribe to this podcast and stay up to date on all the latest AiArthritis news and events.
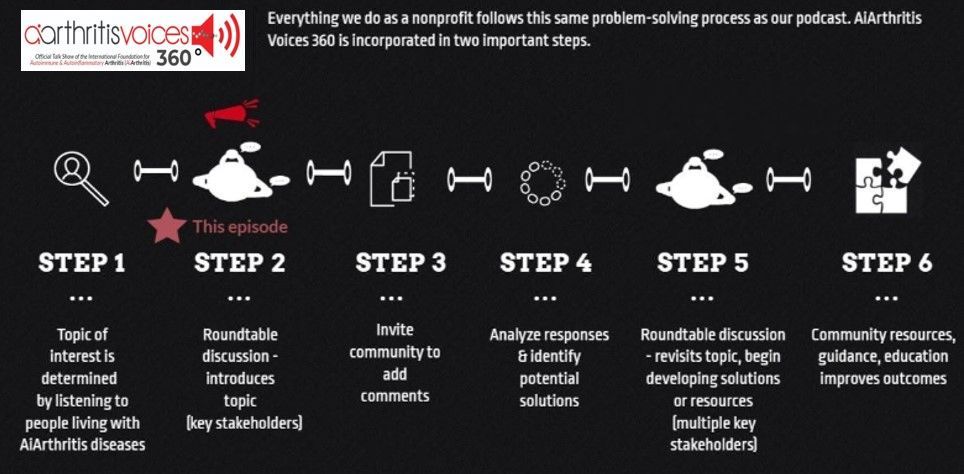
All our main 1st Sunday of the month episodes are either an initial "put the topic on the table" episode (Step 2 in our organization's 6-step problem solving process) or a "revisit to the table" episode (Step 6 in our organization's 6-step process), where we build on a past show because we have moved forward in developing help, tools, or projects around the issue (Step 5 in our organization's 6-step process).
After each show airs we spin off the conversation into many discussions over various formats, which we now call #360its.
-
Additional Resources & Information
- Explore more from the “Go With Us to Conferences” program: www.aiarthritis.org/conferences
- Volunteer with AiArthritis : https://bit.ly/AiArthritisVolunteerApp
Tiffany Westrich-Robertson
Tiffany is the CEO at AiArthritis (International Foundation for Autoimmune & Autoinflammatory Arthritis) and uses her professional expertise in mind-mapping and problem solving to help others, like her, who live with AiArthritis diseases work in unison to identify and solve unresolved community issues.
Connect with Tiffany:
- Facebook: @tiffanyAiArthritis
- Twitter: @TiffWRobertson
- LinkedIn:
@TiffanyWestrichRobertson
Pull up your seat at the table
Now it's YOUR TURN to join the conversation!
What do you think about this episode?
We want to know what you think! By continuing the conversation with your opinions and perspectives - we all get a better understanding of the problems facing our community. Better yet, through these conversations we can start working and developing solutions.
We mean it when say 360. Not only do we want your input anytime and anywhere, but we also are eager to see where the conversation will take us. So please, "pull up a seat at the table" and let's start talking!
Email us at podcast@aiarthritis.org, message us on social media (find us by searching for @IFAiArthritis)
Relevant Episodes & Projects
Blog Post:What Is Undifferentiated Disease (UD)?
Undifferentiated disease refers to conditions where individuals exhibit symptoms resembling those of autoimmune or autoinflammatory diseases, but the symptoms are not specific or severe enough to warrant a definitive diagnosis of one of them. Learn more in this blog post.
#ACR21 Debrief #3 (CLIP)- Undifferentiated Connective Tissue Disease: Need for Recognition
In this debrief, Tiffany debriefs the team on the session she saw related to UCTD and the need for recognition.
Go With Us to EULAR 2023 - Ig-G4, UCTD, RMDs and the Brain
Join us as we attend the 2023 European Alliance of Associations for Rheumatology's (EULAR) Congress of Rheumatology, otherwise known as EULAR 2023.
Love the show? Help us make sure we stay on the air by making a donation.
Your contribution helps us continue the work we do every day to improve the lives of millions worldwide.