Breaking Down Relapsing Polychondritis (RP)
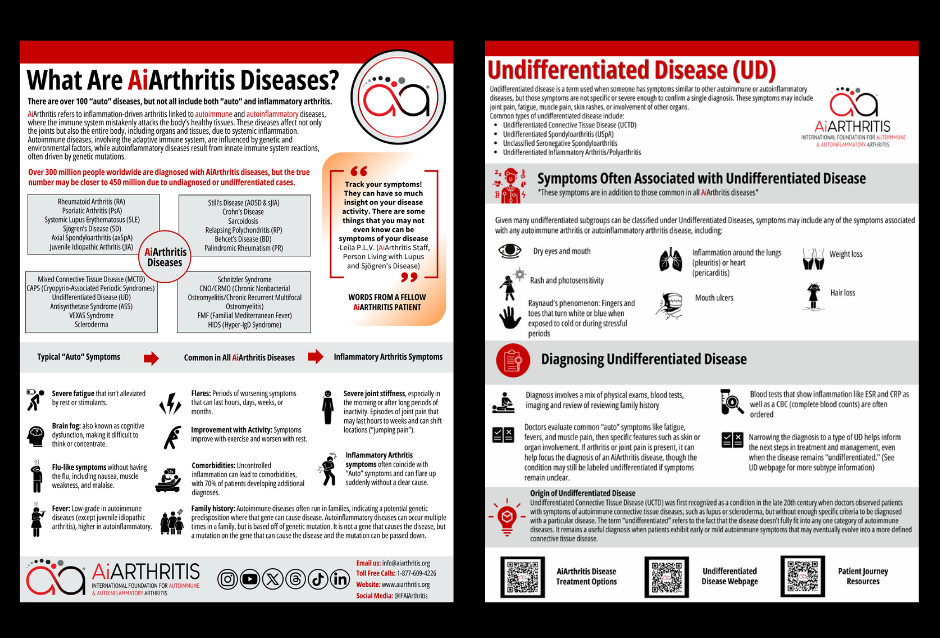
AiArthritis Disease Symptoms
AiArthritis diseases share common features such as flares, where symptoms worsen for hours to months, and improvements with physical activity, while rest can make symptoms worse. Genetic predisposition or mutations can lead to these conditions running in families, and uncontrolled inflammation often results in comorbidities, affecting 70% of patients.
Key symptoms include:
- Severe fatigue that persists despite rest or stimulants
- Brain fog, making concentration difficult
- Flu-like sensations like nausea and muscle weakness
- Low-grade fevers (higher in autoinflammatory diseases)
- Joint stiffness, especially in the morning or after long periods of inactivity
- Sudden, shifting joint pain that starts and stops abruptly
What Are The Symptoms of Relapsing Polychondritis (RP)?
The condition can range from mild to severe, with symptoms varying widely between patients:
- Ear Problems - The earliest sign is often ear pain and inflammation. In severe cases, cartilage breakdown can lead to floppy or "cauliflower" ears.
- Facial Changes - Cartilage deterioration can cause the bridge of the nose to collapse, creating what's known as a "saddle nose" deformity.
- Joint and Body Pain - Many patients experience arthritis-like pain throughout their body, particularly in their hands, knees, and other joints. Some also report discomfort near their breastbone and ribs.
- Eye Issues - Eye inflammation ranges from mild irritation to severe conditions like scleritis or uveitis, which can threaten vision if left untreated.
- Respiratory Complications - When RP affects the airways, patients may struggle with breathing or swallowing. In severe cases, this can become life-threatening.
Additional Symptoms
- Hearing problems and balance issues
- Nasal congestion
- Skin rashes
- Fatigue and fever
- In rare cases, heart, kidney, or nervous system involvement
The severity of RP determines its impact. Mild cases may feature brief flare-ups with manageable symptoms that respond well to over-the-counter medications. Severe cases often require aggressive treatment and careful monitoring by specialists, as they can lead to serious complications and organ damage.
Even with mild symptoms, early medical attention is crucial for preventing the condition from worsening. Regular monitoring helps catch and address complications before they become severe.
Learn More About Relapsing Polychondritis (RP)
Diagnosis of Relapsing Polychondritis (RP)
Diagnosing RP can be challenging due to its nonspecific symptoms and rarity. There is no definitive test for RP, and diagnosis is typically based on clinical evaluation and the presence of at least three associated symptoms over time. Imaging studies and blood tests may be used to rule out other conditions. Here's an overview of the diagnostic process:
- Clinical Evaluation: The diagnosis begins with a thorough clinical evaluation, including a detailed medical history and physical examination. The doctor will look for characteristic symptoms such as ear pain, nasal changes, joint pain, and eye inflammation.
- Diagnostic Criteria: Two sets of criteria are commonly used to diagnose RP: the McAdam criteria and the Damiani criteria. Both require the presence of specific clinical features over time. For example, the McAdam criteria require at least three of the following features: recurrent episodes of auricular chondritis, nasal chondritis, respiratory tract chondritis, ocular inflammation, and arthritis.
- Laboratory Tests: While there is no specific blood test for RP, certain tests can help rule out other conditions and support the diagnosis. These may include:
- Erythrocyte Sedimentation Rate (ESR) and C-reactive Protein (CRP): To measure inflammation levels.
- Antinuclear Antibody (ANA) Test: To check for autoimmune markers.
- Comprehensive Metabolic Panel (CMP): To assess organ function.
- Imaging Studies: Imaging studies such as X-rays, CT scans, or MRIs may be used to assess the extent of cartilage involvement and rule out other conditions.
- Biopsy: In some cases, a biopsy of affected cartilage may be performed to confirm the diagnosis and rule out other conditions.
- Exclusion of Other Diseases: Since RP is a diagnosis of exclusion, doctors will rule out other well-defined connective tissue diseases such as lupus, rheumatoid arthritis, and scleroderma.
- Monitoring Over Time: Regular follow-up and monitoring are essential to track the progression of symptoms and adjust treatment as needed.
Discover More Of Our Resources
Treatment for Relapsing Polychondritis (RP)
Treatment for RP focuses on managing symptoms and preventing complications. This may include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids: To reduce inflammation.
- Immunosuppressive Drugs: Medications like methotrexate, azathioprine, and mycophenolate mofetil may be used to suppress the immune system and reduce inflammation.
- Biologic Agents: In severe cases, biologic agents such as rituximab or infliximab may be considered to target specific parts of the immune system.
- Lifestyle Modifications: Avoiding triggers, maintaining a healthy lifestyle, and regular monitoring by a healthcare professional.
- Supportive Care: Physical therapy, counseling, and support groups to help manage the condition and improve quality of life.
Who Treats Relapsing Polychondritis (RP)
Relapsing Polychondritis (RP) is typically treated by a
rheumatologist, a specialist in autoimmune and inflammatory diseases. Rheumatologists have the expertise to diagnose and manage complex conditions like RP, which involve inflammation of cartilage and other connective tissues.
In some cases, a
multidisciplinary team may be involved in the treatment, including:
- Otolaryngologists (ENT specialists): For ear and nasal symptoms.
- Ophthalmologists: For eye inflammation and related issues.
- Pulmonologists: For respiratory tract involvement.
- Cardiologists: If there are heart-related complications.
Collaboration among these specialists ensures comprehensive care and management of the various symptoms and complications associated with RP.
Prognosis of Relapsing Polychondritis (RP)
The prognosis for RP varies. Some individuals may experience mild symptoms that respond well to treatment, while others may have more severe and persistent symptoms. Regular follow-up with a healthcare provider is essential to monitor the condition and adjust treatment as needed.
Relapsing Polychondritis (RP) is a complex and rare condition that requires careful management and monitoring. Understanding the symptoms, causes, and treatment options can help individuals with RP and their healthcare providers develop an effective management plan.
Related Blog Posts
November 29, 2025
Having multiple health conditions when living with an AiArthritis disease is not uncommon, discover why and what conditions are common.
July 16, 2025
Learn more about World Sjögren’s Day.
June 26, 2025
Discover more about Chronic Disease Awareness Day and why it matters.
Show More