"Accumulator" and Access to Treatments
The "Accumulator" is an issue within the US healthcare system that can affect treatment availability and access -
but our solution can impact education and access globally.
How would losing access to treatments affect your ability to work?
Submit Your Testimony
This access issue is relevant for people in any place in the world, even though the "Accumulator" is US.
If you are a patient using biologics or similar disease-modifying agents, and you would like to share with governments, legislators, and employers how losing access to these treatments would negatively impact your ability to work, we want to hear your story. These testimonies will be used to fight for patient access to treatments.
Current access to treatments process for those living in the US and who have private insurance or plans through their workplace.
In the United States, most patients use drug manufacturer copay discount cards to help them afford their biologic or specialty medications - which can cost thousands of dollars out-of-pocket a month. If the patient has health insurance, they will have what is called a copay, or the amount of money they must pay per prescription. They also have what is called a deductible; this is the grand total that they have to pay out of pocket before the insurance company will pay for 100% of their prescriptions. Many deductibles are thousands of dollars.
So let's say the amount a patient has to pay out-of-pocket before insurance coverage kicks in (their deductible) is $6,000 usd. And their copay amount, or the amount out-of-pocket they have to pay for a prescription until that deductible has been met, is 30%. If a drug costs $100, then 30% may be reasonable ($30). If a drug costs $2,000, many people could no longer afford it ($600), so they would go without. If they did pay it, they would need to still pay it for as many months as it took (in combination with other out of pocket treatment costs) to reach the $6,000 before insurance would cover the drug. To help patients, manufacturers created "copay assistance cards". Since the monthly cost of having insurance is also expensive (example $600 a person a month), these cards help patients meet their other plan costs and still gain access to treatments.
But many insurance companies and pharmacy benefit managers (PBMs) are adding copay accumulators to their insurance plans. This simply means that those copay assistant cards can no longer be applied to the patient’s deductible (or the amount of out-of-pocket costs they have to pay before the insurance kicks in).
Who will this impact? This will mostly affect patients with high deductibles and those who get their insurance through their workplace - as there are cost benefits to companies who choose these plans. So what can we do?
The Solution
One way this issue is being addressed is through the great work by many nonprofit organizations who are advocating for legislation that prevents accumulator programs from causing patients to lose access to treatments. We are part of the largest US coalition addressing this issue, led by the Arthritis Foundation.
Drug manufacturer's have also switched to credit cards instead of discount cards. Patients are given these cards and call the manufacturer's assistance program periodically to have it loaded with funds.
Our organization is also is working on a solution that we believe can help the work being done in the coalition:
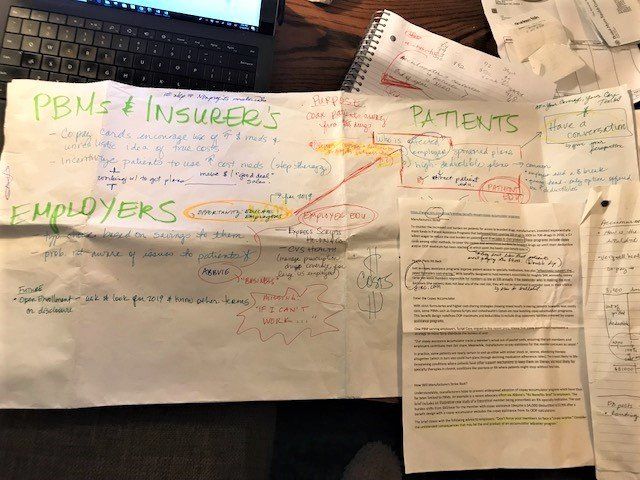
In 2018, we investigated current efforts to address this situation, in an attempt to determine which groups are being affected most, what is currently being done to solve the problem, and identify any way the addition of patient voices could trigger a different solution.
Given most nonprofits are already addressing patient education, and what to do if you have a high-deductible plan, we decided to focus in on those patients who have employer sponsored insurance plans. We noted that while some pharmaceutical companies have worked to educate Human Resources (HR) staff about what the accumulator is, no one is sharing stories from people who rely on these treatments to be able to work and how losing access would impact their lives.
Examples include:
- Pain, inability to do regular tasks, may not be able to be at work for same duration, more doctors’ visits, more days off
- Brain fog, inability to think clearly, complete tasks
- Late for work (stiffness)
- Need for remote office accommodations and in office accommodation
Collecting stories from patients PRIOR to this happening, and sharing it with HR departments, we believe, is key to demonstrating our need for access - and what the company would be responsible for happening to their employees if they choose plans that remove that access.
We also believe these same stories could be used for legislative purposes. So in 2019 - 2020, we are collecting testimony from patients who rely on treatments to remain in the workforce. This data will be provided to members of the accumulator coalition we participate in, hoping that it can influence our impact.
How can this have global impact if it is addressing a US insurance issue?
There are access to treatment issues all over the world, whether that be due to insurance or government or geography. Collecting patient stories that explain what could happen if access to treatments was no longer possible could influence legislation world wide. Why wait for "this happened to me" stories to try and move the needle? Patients should have to suffer first in order for action to be justified.
How would losing access to treatments affect your ability to work?
Submit Your Testimony