#MyStills Campaign
Learning from Our Journey
Vanda's Story
Vanda is from the UK/Hungary and is diagnosed with Adult Onset Still's Disease.
"I was probably mis-diagnosed with Juvenile Rheumatoid Arthritis when I was about 5 but knowing what we know now, it was more likely either PFAPA or Systemic Juvenile Idiopathic Arthritis (the childhood version of Still’s). After having my tonsils removed at 13, I went into total remission and I lead a completely healthy life for 20 years. As an adult, my initial symptoms came on suddenly last year, following a small laparoscopy surgery, and initially resembled a bad infection. Doctors thought first that it was a post-surgical infection and I was given lots of antibiotics. I began by getting odd aches and pains, then daily fevers where I’d have a low grade fever during the day and extremely high fevers at night. I had chills, shivers, I would wake up drenched several times at night, and with the fever came often unbearable pain too all over my body. I felt weak and incredibly fatigued - like I have never had a good night’s sleep. At the time I explained this like feeling like I have just run a marathon and then had a few rounds in the ring with Mike Tyson. My neck then completely seized up, I had constantly sore throat (but no visible throat infection), random evanescent rash on my torso and inner thighs that came and went and often had various joints swell up too. Things got so bad that I couldn’t make it up or down the stairs in our house, couldn’t get my youngest in and out of the car, couldn’t even carry my work bag or walk much. I spent nearly three months going back and forth between my GP, then a rheumatologist and had three trips to the A&E before `i was admitted to hospital. In hospital I had every test imaginable. Xrays, CT scans, MRI, PET scan, lumbar punctures, blood tests several times a day, ultrasounds, and many more. I developed pericarditis and then pleural effusion too. By the time we ruled out exotic infections, we were left with either a diagnosis of a rare disease or lymphoma."
Aukje's Story
Aukje is from the Netherlands and was diagnosed with Adult Onset Still's Disease in 2019.
"I experienced my first symptoms exactly one week after moving into our new home. My knee and one finger became extremely painful out of the blue. That night, I got a fever, a rash all over my body, and all my joints had become painful. At first, I thought I had become ill as a result of being extremely busy, but my GP was worried and didn't understand what was wrong with me. The test results of my dermatologist were inconclusive, and prednisone only helped to get the fever down. After a week of high fevers and no one knowing what was wrong with me, I became very worried and anxious. When my rheumatologist finally mentioned Still's, I was relieved to hear what was wrong with me. The fact that Still's doesn't have a cure doesn't bother me. I have relatively mild symptoms, and eight months after my first flare-up, I can live my life pretty good, and appreciate it more."
Catherine's Story
Catherine is from Ireland and was diagnosed with Adult Onset Still's Disease in 2017.
"In September 2017, I was diagnosed with Onset Adult Still's Disease. I was 49 years old at the time.
I returned from a holiday in Mexico and was feeling unwell. I was very tired, had no energy, a sore throat, and a headache lasting approximately three weeks. I thought I had not been sleeping either. My doctor was away, and a sub doctor said I had a virus and gave me sleeping tablets to help with the sleep. After a few days, I developed sore eye sockets and itchy hands. Over the weekend, I was sweating profusely and, I developed a rash around my stomach area. When I went to the doctor on Monday morning, my wrist was so sore, I thought it was broken. My doctor said my heart was racing when I was sitting, like I was running, and said he did not know what was wrong with me. Because I had been away, he said he thought I had Zexa or Sars, but it looked like Meningitis. He advised me to go to the hospital for some tests.
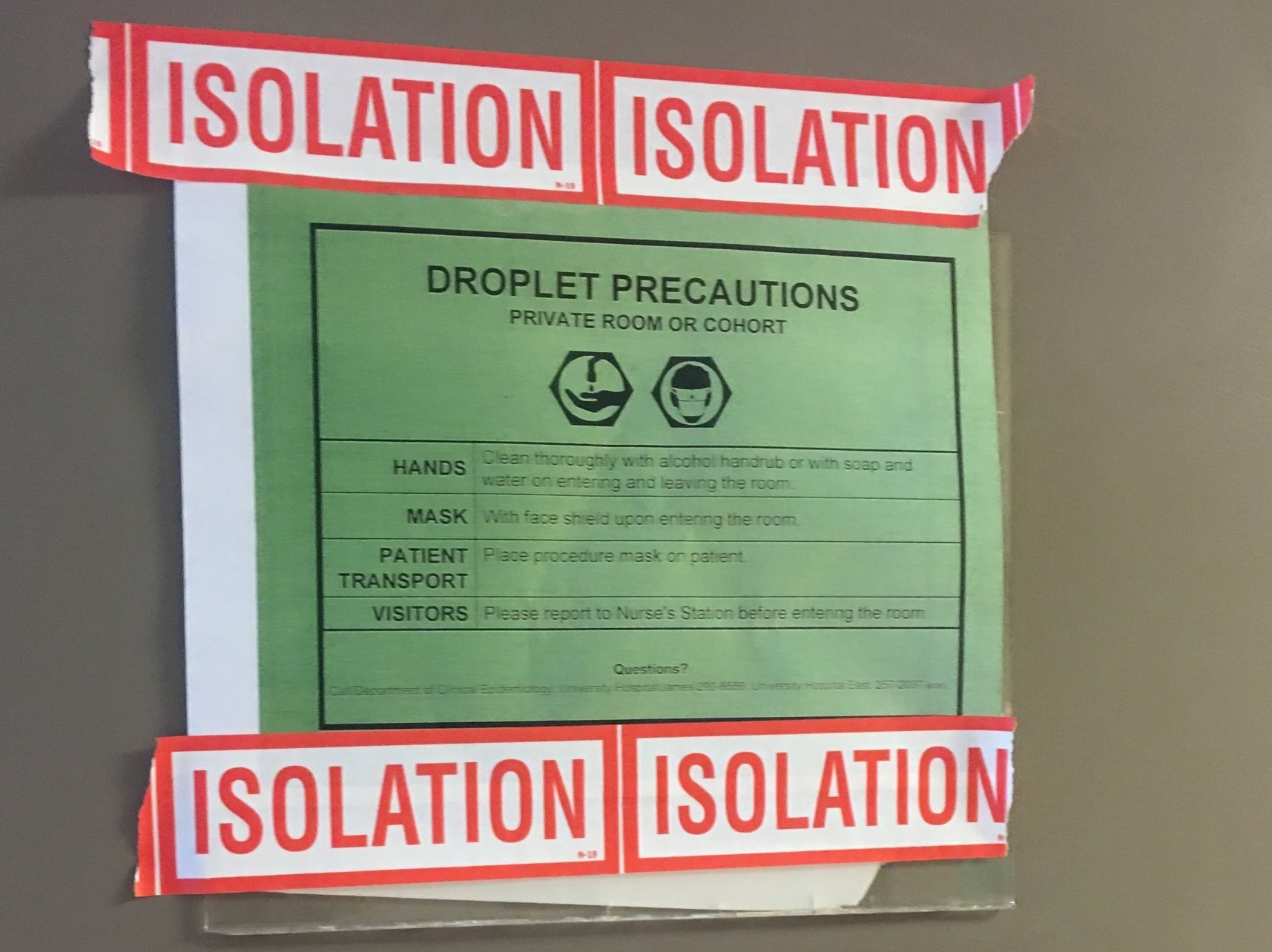
I went to the hospital. Later that day, I transferred to another hospital that would know more about infectious diseases. They did not know what was wrong either, so they put me into isolation.
After teams of people came to see me after three days, a young doctor said he had read about Still's before. As my rash was coming and going and I was sweating now (like bedwetting sweat) twice a night, he asked the Rheumatology team to see me. After a discussion, they decided that I had Still's.
I was terrified, to the extent that I thought I was going to die. When told I had Still's, I did not believe it. I wanted to know more, but I couldn't find much about it. I felt confused and like my world had turned upside down.
When I came home from the hospital after three weeks, I felt like I was hit by a bus. I wanted to do things like housework and go for a walk, but my energy would not allow that. I was now suffering from anxiety and I wanted to find someone else that had this, but I could not find anyone else. I felt alone."
Claire's Story
Claire is from Ireland and is diagnosed with Adult Onset Still's Disease.
"I had been feeling unwell for 6-8 months before becoming very ill in May 2016. The terrible fatigue I was feeling was due to moving house and work stress. When I felt unwell in May, the GP was sure it was just bad flu, but my temperature was ongoing over days, and I felt increasingly sick. I knew I was very unwell. I asked to be admitted to the hospital and was, at that point, considered critical. My symptoms were high-fevers and shivering, rash, pain in wrists, pneumonia in both lungs, and sore throat. I was very unwell, and it took the doctors a number of weeks to diagnose me. I was released from the hospital 27 days later and began a long journey of recovery. I was two years out of work and started learning all I could about this disease.
What a rollercoaster! At first, it looked like I had stage four Lymphoma, so an autoimmune illness diagnosis after this felt like a relief. I had a small child and wanted very much to be here for her growing up. Having been critical in the hospital and feeling like I was very close to death (I was also diagnosed with MAS ( Macrophage Activation Syndrome)), my emotions were raw. I felt that it would be a long path to recovery. It certainly was."
Adele's Story
Adele is from the UK and is diagnosed with Adult Onset Still's Disease.
"In February 2016, I started to become unwell on the run-up to my wedding. At first, I thought I had caught a virus from my soon to be husband who had been away on his Stag do when he came home with an awful virus. My first symptom was a rash on my hands, and it soon spread to the rest of my body. I then started getting a fever, a sore throat, and then swollen joints on both knees, ankles, hands/wrists, and hips. I had an extremely sore throat and a rash that would appear and was extremely itchy. My temperatures were extremely high, I would have to change my night clothes through the night, and I’d have to put a towel on the sheet. I was extremely exhausted and was sleeping a lot.
I went to the doctors where they thought I had an allergic reaction and gave me some prednisolone (25mg per day). The closer I got to my wedding date, the worse I became. My dad took me to A&E. They examined me, but didn’t take any blood. They felt it too was an allergic reaction and increased my prednisolone to 30mg. I was bent over double, and my dad said I shuffled like an old lady. I couldn’t get any footwear onto my feet as they were so swollen. I booked an appt to see my local doctor and I was in tears climbing the stairs to his room. He met me at the top and my Mom, who had come with me, said Dr please we need to help her, she’s in agony, she has her wedding tomorrow. He said he wanted my inflammatory markers checking but didn’t want to do them that day as he said I would have needle marks on my pictures. His reason for not taking blood is that he felt I wouldn’t get to have my wedding day as he thought they’d keep me in taking a look at me. He gave me a high dose of painkillers, ibuprofen, and paracetamol.
I got through my wedding day, albeit in agony. My rash made an appearance in the afternoon, and as the day wore on, my temperature kept rising. My cheeks were so red by the evening. I took my tablets throughout the day, my husband had to cut up my food as I couldn’t, and I couldn’t hold the pen right to sign my name in the register. But, I enjoyed my day thoroughly, probably through adrenaline surging around my body.
The next day I woke and I couldn’t physically move, I was in so much pain. I couldn’t lift my leg to get it into the shower over a bath. I got down to breakfast, and I couldn’t lift my head off the table or bend my elbows to put food to my mouth. My parents and my husband were so worried, my husband took me to A&E that afternoon, and they kept me in. They ran lots of blood tests. The A&E doctors were so baffled that they came up to see me in the ward two days after as they were fascinated with me! They tested me for rheumatoid arthritis, but it was negative. Two days after, they sent me home asking me to reduce the prednisolone by half, down to 15mg. I did what they said, and they got an appt to see rheumatology as an outpatient. The following Saturday, a week after my wedding, I started coughing up blood. My husband took me back to A&E where they kept me in for four weeks. They gave me a steroid shot, but stopped all meds to do loads of tests.
My temperature was getting up to 42 degrees, and I had to have my bed linen changed 3-4 times a night as I was dripping with sweat. After about ten days, a rheumatologist and infectious diseases doctor came and said they felt I had fluid around my heart, and my spleen and liver were enlarged. They thought it was either Still's or Sweets syndrome. They had my ferritin checked, which was then the deciding reason they diagnosed Still's. My ferritin was 11700, CRP 267. They also tested me for Lyme disease, cancer, rheumatic fever, sepsis, but all came back negative. They put me on 60mg prednisolone and wouldn’t allow me to leave until my temps came down.
I had to go back to my parents as I couldn’t walk. I had a nearly 2-year-old daughter to look after, and my husband works away, so I spent three months convalescing at my parents.
I went to the National Amyloidosis Centre at the London free hospital to see their specialists. They did other tests for autoinflammatory diseases and agreed I had Still's. With my levels being so high, they had concerns I had the starting of macrophage activation syndrome. I was distraught since I had just gotten married and I was scared, but mostly I wanted to feel well again! I had just started on a journey with my new husband and felt like the illness got in my way! I also felt depressed that we couldn’t go on our honeymoon and I couldn’t walk. I was also angry that I depended on my family so much. I am a very independent person and felt I was a burden."
Amanda's Story
Amanda is from the UK and was diagnosed with Systemic Juvenile Idiopathic Arthritis at age 5 and was diagnosed with Adult Onset Still's Disease in 2018.
"I had whooping cough at age 5. As I was feeling unwell, I was lounging on the sofa and started complaining that I was unable to move my elbow. The doctor thought it was because I had not been moving. The next morning, I awoke crying out in pain at the blanket touching me. My knees were very swollen and red, and I was unable to move. I was admitted to a local hospital and then moved to a London hospital with the specialist at the time Dr. Ansell. I was diagnosed with Still's Disease at the time, which started being referred to as sJIA. My main symptoms were that of arthritis, and I had ongoing joint damage and issues into adulthood. I was primarily treated as though I had RA. In 2018, I had a sore throat, all over body pain, rashes, fevers/rigors, full-body edema (6kg of it), skin stretched to a splitting point, and I became incredibly unwell. I was admitted to the Acute Respiratory Care Unit, unable to move or swallow with a CRP of 603. High CRP count meant that this was dismissed as a rheumatology issue (as they said that they would not expect to see a count above 80). My rash was confused with an allergic reaction to antibiotics, and I was treated as having sepsis. I kept saying that the rash reminded me of the one I had as a child.
The rheumatology consultant eventually saw me and acknowledged that this was AOSD. Raised ferritin levels (although not above 10,000) and my subsequent response to medications confirmed it. I don't remember initially as a child. I remember feeling fed up at being unable to do what other children were doing. I felt like I was being treated like a baby since I had to be carried into school when unable to walk and had to urinate in a potty to have urine dipped when having gold injections. Growing up, I had a pragmatic approach and felt that I just had to get on with it and manage to lead as full a life as possible. I always looked at it as a physical mobility/pain issue that could be dealt with surgery. My more recent flare has been much more challenging and has meant that I have had to face my own mortality, and I have found it more challenging to be stoic about my condition; however, I continue to try to maintain this approach as best I can."
Natalie's Story
Natalie is from Australia and is the parent of a child with Systemic Idiopathic Juvenile Arthritis. Her story is about her daughter's journey to diagnosis.
"My daughter's first symptoms were subtle at the beginning. It started with a fever and a swollen red throat. The rash came next. She was four months old, wasn't gaining weight, and she wasn't growing very fast. She was on antibiotics month in and month out because we kept getting told that she had a virus repeatedly. By the time she was eight months old, her fever pattern was predictable. I was getting up eight times a night to help her turn over or change position because she was in too much pain to move. I knew something was not right. Finally, we saw a pediatrician in town (who had already retired when the symptoms started), and she told us to take our daughter to the hospital. She would call ahead. Our daughter was hospitalized for 13 days in a small town near our village in France. She wasn't doing very well, so she was sent to the big children's hospital in Paris. This is where we received the diagnosis of Still's disease.
Before the diagnosis, we were frustrated and scared. Frustrated because we knew something was wrong, but there were no answers. After the diagnosis, we felt relief. Finally, we knew what was wrong, so a plan was put in place to relieve her pain."
Tammy's Story
Tammy is from the United States and her relationship to Still's disease is a parent/caregiver relationship. Her story is about her son's experience.
"My family's journey with Still's started in April of 2016. My son Ronnie developed a skin rash that covered the majority of his body. This rash appeared to be like an allergic reaction to what we thought was his new prison guard uniforms. He went to the emergency room and was given steroids for the rash. He was asked the typical questions like 'have you changed laundry detergent' or 'been around poison ivy' and so forth. None of those were the cause. The steroids did very little for his rash. After about a week, he started having more symptoms that included fatigue, fever, aches in his limbs, and so forth. He went to the emergency room again, and they started testing him for all sorts of things. Everything kept coming back negative. They could not figure it out, so they sent him to an infectious disease doctor who started testing for more severe diseases, which again all returned negative. He was admitted into the hospital for observation after he began having nausea and vomiting and continued high fever. He was in the hospital for eight days with no diagnosis. They sent him home with more steroids and antibiotics.
He continued to feel worse, but did not want to go back to the hospital because they couldn’t figure out what was wrong. He would rather feel bad at home than at the hospital.
Over the next week, we watched him slip away. He continued with fevers and nausea, zero energy, sore and aching body. He went the day before his next doctor's appointment to get blood work done for the appointment. He was so weak and sick that he barely was able to do this.
The doctor called first thing in the morning and said he was in renal failure to get him to the emergency room immediately. Before he could leave the house to go, he started seizing and was transported to the hospital via squad. Upon arriving at the hospital, the doctors had no idea what was going on and why. They just said if he doesn’t settle down, his heart will explode. He seized for over an hour until they were able to give him medicines to calm down. He was then life-flighted to a larger hospital. After about 20 minutes at the new hospital, he coded twice, and the doctors were able to revive him. Over the next 24 hours, his body began to shut down, one organ at a time. There are many details and things that happened, but I will take the time to mention the most significant at the moment. His kidneys shut down, and they put him on dialysis. Then his blood pressure needed to be stabilized, which they maxed out three medications trying to do this. They said if he made it through the night, he might have a chance. He did make it through the night, but the next day was horrendous. They iced his body to bring the temperature down to try and save organs. He went into macrophage activation syndrome, which we know now, but at the time did not have a clue of what was going on and why. The doctors just stood and watched dumbfounded as to what and how to help him. His spleen was enlarged, his liver went bad, his stomach started bleeding internally, he lost brain function, and then the doctors advised us that if we shut off his blood pressure meds, he would probably pass. We decided to let him pass, and 45 minutes after turning off the meds, he passed. However, they had to raise his body temperature before they could pronounce him dead.
So long story short, he was NOT diagnosed until after his autopsy report came back. The doctors had no clue what they were dealing with. My son was sick for less than 30 days. He was always healthy and active. Never had any health issues, and no indicators of such an illness would take his life at the age of 20. Had the doctors known about Still's and how to treat it, my son may still be with us."
Lisa's Story
Lisa is from the United States and was diagnosed with Adult Onset Still's Disease with Juvenile Onset in 2016.
"I was first diagnosed in June 2016, when attending Realtor school. It started with hives and severe itching, and no medicine was helping. After a week of having hives, I started getting red-patchy-like rashes on my chest, then arms, and finally legs. My eyes began watering severely so much so that I had to carry a box of tissue around with me.
After going to class with no makeup and hives from hell, I woke up one morning, and my legs were in severe pain, and I couldn't stand on them. I called my doctor's office, and they said to either call an ambulance or get to E.R. NOW! I went to the hospital, but they had no idea what was wrong with me. They just knew my lab work meant I was a sick person. I stayed in the hospital for two weeks.
The first week I saw every doctor they had and no answers. I asked to go home, but that didn't last long. I went home, laid on the couch, and my daughter stayed with me. In the middle of the night, I tried to go to the bathroom, but I fell because I couldn't stand. I was hoarse and couldn't speak much, so I threw a book at my daughter to wake her up and get my husband. He called 911, and the ambulance took me back to the hospital.
I felt like I was a burden to them, as they wanted to pass me off to a rehab facility but with no diagnosis. My husband and sister were so upset at the suggestion. They made room for me for another week and tested for many things before finally coming up with Still's Disease.
I wanted a second opinion, so my husband took me to the Mayo Clinic in Scottsdale, AZ. After running a series of tests, I was told I had this since I was a child. I did have pain problems in my legs and back, so the doctor said it was developing as I was growing. But because no one knew what Still's was back then, it didn't get diagnosed."
Lana's Story
Lana is from the UK/Canada and was diagnosed with Adult Onset Still's Disease in 2018, but is now in remission.
"I was diagnosed in August 2018. My first symptoms were achy joints, especially my back and knees. I remember going to see my GP, and he told me that my aches and pains were due to getting older and all the impact that my running and weight training was doing on my body.
At the time, I started to feel the aches I was 47 years old and in good health. I was waking up with a painful back and my knees hurting. I would have to take Advil and other over the counter drugs to help me cope with the pain. I had then gone to see a physiotherapist who referred me to an Osteopath. It was my Osteopath who said that with the reoccurring aches and pains I was having, I should look into seeing an Arthritis specialist. I was having trouble sleeping and was so depressed.
About six months into all the aches and pains, I noticed a small red round rash on my right hip. Within a few days, the rash moved to my buttock, then chest and then my arms.
When I went back to my GP, he got me an appointment with a RA specialist. When she saw me, she right away diagnosed me with Still's disease. Once I got the rash, all the other symptoms came into play really fast. All my joints swelled up, and I went to emergency. It was there that they did my blood tests and all the results pointed to Stills. I had low-grade fevers every day that would come and go, and the rash was all over my body. They right away put me on 60MG of Prednisone. Once I was on Prednisone, my symptoms slowly got better, I could walk, and my swelling of the joints started to go down."
Ana's Story
Ana is from the United States and is diagnosed with Adult Onset Still's Disease.
"My first symptoms started in September 2015, 3 months after I gave birth to my daughter. It began with a severe rash that would appear in the morning, with only a few spots here and there, all over my arms, back, and legs. By the end of the day, my whole body would be full of rash. The rash was not itchy, which surprised everyone because they thought it was an allergic reaction to something. In addition to the rash, I had severe pain in all my joints. My joints were suddenly swollen, from my finger to my knees. This made it hard to take care of my 3-month-old; however, I managed to get it done.
I was finally diagnosed about two years after the first symptoms showed up. It took a while because, for one, they had to do a lot of tests, as you may be aware. When my symptoms first started, I went to the emergency room. They treated it as an allergic reaction and gave me meds, which didn’t do much. After 3 or 4 months of having really bad with symptoms, everything went away as if nothing happened. My husband and I thought I was better, and life went on.
Then about springtime, April to be exact, all the symptoms came back, and it was worse. Severe pain and swollen joints, rashes everywhere. After a day of terrible pain, I want to emergency again. I thankfully never had to be hospitalized. They prescribed prednisone which, as you may already know, helped immensely. Because I took care of the baby and worked full time, I always made excuses not to go and see a doctor. I eventually decided to go and see a regular doctor around my birthday in November. She sent me to get blood work done and then sent me to a rheumatologist because she knew it was out of her expertise. Once I met my rheumatologist, we did test after test, many more since I work as a vet assistant. It took many months, and my husband was researching since she had no idea what was wrong with me. Finally, my husband asked about Adult Still's disease. She said, 'Hmm, everything else came back negative.' They tested for Still's, and I was informed I had Adult Onset Still's Disease when I turned 40, but I started all this when I had just turned 38."
Kari's Story
Kari is from the United States and is diagnosed with Adult Onset Still's Disease.
"My symptoms came all at once out of nowhere but presented the same each time I flared. I would wake up from a dead sleep with severe right flank pain, fever/chills swollen lymph nodes, nausea, and chest pain. Pain that was sharp and made it difficult for me to breathe. I had the faint salmon color rash on my inner thighs and chest, but I didn't think anything of it back then. I thought it was from my fevers. These symptoms started when I was around 12, which would happen to me about once a year. Then as I got older, it progressed from "flaring" every 12 months to every six months to every month to multiple times a month. All I wanted was to live my life, and this was preventing me from doing so.
Looking back in my medical history, I started having weird symptoms when I was one year old. I always was sick as a kid with what they thought was strep throat since my tonsils were so large. I had my tonsils out when I was ten, and that seemed to help with my sickness until I was 12. I would be taken to the ED because of my fever. There I would be pumped with all kinds of antibiotics because I presented with what looked like early sepsis. My labs would be the same every time (I know this because my mom and I collected all my medical records and graphed how many times I was in the hospital and my lab trends). The lab results showed WBC high, sed rate and CRP high, and ALT and AST high. I would go through the ED and be admitted for one week at a time. I was consulted by cardiology, and my heart rate was all over the place. Baseline I run 60's; when I flare, it can get as high as 220s.
I had to wear multiple heart rate monitors. I have had multiple echos, EKGs, etc. to follow up on my chest pain. I was prescribed a beta-blocker, which I don't take. I have been consulted by ENT, infectious disease, OBGYN, nephrology, and hematology/oncology. I have always had to follow up with infectious diseases because I would always be discharged home with no diagnosis. At one point, since my symptoms started when I was younger, my pediatrician saw me, she told my parents I was seeking pain meds. I was in so much pain each time I flared. Pain meds would take the pain away for a little bit, and then it would come right back.
When I finally got my diagnosis, I wrote her a letter stating to look outside the box and not try to fit everyone under one label, but she never responded to me.
I finally got my diagnosis when I took my health into my own hands. My last hospital admission, which they tried to discharge me home from the ED, I said no because my fever was 102, and my heart rate was in the 180s, which is abnormal for me. They said, 'ok, we will monitor you overnight.' I got progressively worse overnight. They monitored me for a week, per usual, I saw the usual slew of doctors except I demanded they bring in a rheumatologist. They had to consult outside the hospital because there were no rheumatologists at this hospital. The rheumatologist took one look at my labs and me and said I haven't seen this outside of med school, but I think you have Still's Disease. I did some further lab testing, which all fit into the Yamaguchi criteria. I also had to do a lymph node biopsy to confirm I did not have cancer or leukemia. As I have gotten older, I have had the associated joint pain and swelling when I flare. I have been to 4 hospitals total to seek care, one of which was Cleveland Clinic to confirm my diagnosis."
Karen's Story
Karen is diagnosed with Adult Onset Still's Disease.
"I had no insurance (self-employed), so when I initially got sick, I assumed it was a bad flu, so I waited a few weeks to get better. When this didn’t happen, I went to a family practitioner that was stumped & wanted me in the hospital. I didn’t go because 1) no insurance and couldn’t afford a hospital stay. 2) my misunderstanding, denial, and stubbornness that this would go away. I had never known anyone with a chronic illness. Any sickness I had ever seen was acute, went through its stages, and went away. That was the only cycle with which I was familiar. Since I wouldn’t go to the hospital, the doctor suggested testing to narrow things down (EKG, etc.) (which were $100’s of dollars at Urgent Care Clinics) and recommended seeing Infectious Disease specialist.
I was immobile. I could barely walk, swallow, and had intense fatigue. I went to Sunday Dinner and saw my parents, who recognized my denial and stubbornness, and they took over where they could. They took me to (and paid the bill) for EKG and got me into various specialists and a top Rheumatologist on the island.
This Rheumatologist declared my illness as Rheumatic Fever and prescribed antibiotics and steroids for my foreseeable future.
The steroids gave me a small amount of imaginary energy to move my life to Texas, where I had a home and an inexpensive cost of living. I started to accept that this was my future health, and I needed to find a place where I could try to be a bit independent. This emotional stress and physical moving just aggravated my illness. The steroids could no longer cover up so many symptoms, but now I was on my own in Texas. Luckily, I had friends around that put in the work to find my medical help. I could not even open a phone book to look up doctors or hold the phone to dial (2005). When I could, I was finding it impossible to even get an appointment with ANY doctor. Many doctors would not see me without insurance (even with the promise of paying cash at the appointment). Any non-profit medical help was not accepting new patients as their patient rolls where overfilled. Those doctors that would consider seeing a cash patient were not accepting new patients.
Amazingly, my friend, Becky, called her Grandmothers doctor, who she liked and asked for an appointment for me. They were not accepting new patients, but Becky didn’t mention that I was new. Apparently, 15 years earlier, when I had lived in Texas and had a job with health insurance, I had been seen at this clinic, and so my name popped up in the clinic computer, and Becky was able to get me an appointment.
At my first visit, the doctor, Dr. Christopher Parker, suspected Still's, but he wanted time to consult with his co-doctors and do some tests before getting back to me because it was so rare. On a Saturday, Dr. Parker called me at home and got me started on methotrexate and had me come back in. At the second visit, he had educational brochures, clear explanations, and an aggressive medical plan. He also got me started with biologics, set up with other doctors in the clinic, started the paperwork for disability and patient assistance programs, and got me on the road to a more normal existence."
Eleanor's Story
Eleanor is diagnosed with Adult Onset Still's Disease.
"My first symptom was a random salmon coloured rash that would come and go on most of my body. I was 24 at the time. In the first instance, I was referred to a dermatologist who couldn't help.
By this time, my joints were hurting, and my wrists were the worst. I was also having fever spikes of 104 twice a day, major fatigue, muscle wastage, and significant weight loss. I was never skinny, but I dropped to 7 stone. I was referred to rheumatology, who was baffled by my symptoms. I was tested for cancer, lupus, and many more. As with most Still's cases, the blood results were different from other inflammatory diseases.
I ended up admitted to hospital, and after six weeks at a multidisciplinary meeting, which included a paeds rheumatologist, they had a light bulb moment where he suggested Still's.
I was put on steroids, methotrexate, and hydroxychloroquine. Finally, over a period of 6-12 months, the symptoms were able to be managed.
During this period, I couldn't get out of a chair, off the toilet, or out of the bath. To this day, I still have to get out of the bath in a certain way due to the damage done to my wrists. Since then, my medications have changed due to my pregnancy with my daughter 16 years ago. I now take azathioprine 175mgs and no other drugs. It keeps the Still's down to a grumble in the background, and stops the fever spikes and rash but is still there and flares up with stress. I am 50 this year, and I have been left with chronic arthritis and Osteoarthritis. I have had a foot fusion, two back surgeries, and the bone-chilling fatigue. I suffer from chest infections and stomach pains occasionally."
Kelly's Story
Kelly is diagnosed with Systemic Juvenile Idiopathic Arthritis at age 6.
"I was born with a rare form of a disease that used to be called JRA (Juvenile Rheumatoid Arthritis). It is now called SJIA (Systemic Juvenile Idiopathic Arthritis) or Still’s Disease. It is an autoimmune/inflammatory disease. I was diagnosed when I was six years and watched my parents get told I wouldn’t make it to my 14th, then 16th, and then 18th birthday. I saw their pain, but I did not understand it. I saw things from a child’s perspective. I was invincible, just like any other kid.
SJIA has affected my life every single day. It caused me to develop severe allergies, asthma, idiopathic seizures, liver problems, inflammation of organs, inflammation of all my major joints, inflammation of the connecting tissues to my muscles, and destroyed my immune system. It has caused me to lose a lot of my eyesight over the years, and inflammation behind my both eyes (a flare-up looks like I was in a fistfight with someone and the side of my face took a pretty bad beating). I developed pleurisy (inflammation around the lungs) and pericarditis (inflammation around the heart). It caused me to develop Fibromyalgia back when it was an “unknown disease” by the time I was 16.
I spent a lot of my life in hospitals, either day clinics once a month at Sick Kids in Toronto or the local hospital or sick at home. I’ve been in a coma for almost a week. I have stopped breathing many times and came so close to not being here. My most severe recent event was two months ago. I am now at the stage where I'm high risk for multiple TIAs (mini-stroke), which could lead to a massive stroke.
Having an autoimmune disease means that I would automatically get a common cold if exposed to it. I had chickenpox when I was 5 for two months. Our family doctor said it was the worst case he had ever seen. I had many allergies, so they decided to do an allergy test. Back in those days, these were done quite differently than today. They would make 1” scratch marks in rows of 10 from your shoulders to your waist. Most people reacted to one or a few of the allergens. I reacted to every single one. I began allergy needles every week. The common practice is to start weekly and then wean to one month, and eventually, the body builds up sufficient resistance to the allergens. This didn’t happen for me, my body could not develop a resistance to the allergens, but the needles kept me alive. I had my needles every week until I was 20 years old when I finally decided to stop getting it.
I watched my parents for my entire life. Growing up at Sick Kids, I watched my parents as they befriended other parents and later learned that their child did not survive. SJIA was a “death sentence” when I was a kid. Many kids are still dying from it. No one knows what causes it, and there is no cure. They now have several types of treatments that they can try. Unfortunately, I’m not a candidate for any of the treatments. One set of medications can kill me, and the other group cannot help me because my immune system is too compromised. As I get older, I become more fearful. I’ve met a handful of other survivors with SJIA who live with the same fears as I do. All of them are in my age range (40s and early 50s).
There is one thing that I have learned living with a rare and potentially fatal disease – life is precious. My parents lived for “today” because they never knew what “tomorrow” would bring. They never knew if the next visit to Sick Kids they would be told I had developed further complications. My Mum taught me that there is a gift that we can all share with others every single day no matter how “hard a day it is” – try to put a smile on someone else’s face. My Mum lived for “today” and put a smile on the face of every person she saw each day, right up to the day God called her home in August 2015. I live the same way. I don’t know why I ended up being one of the “lucky ones.” I guess God has had plans for me, and it’s taken me longer than some of the others whom He called home earlier than me.
We need to find a cure for Still's Disease, for SJIA to make sure more children live to have wonderful adult lives!"
Lisa's Story
Lisa is diagnosed with Adult Onset Still's Disease and Rheumatoid Arthritis.
"I was diagnosed in July 2017 with Adult Onset Still’s Disease at age 53. I had been running daily fevers and experiencing severe fatigue for ten months. I saw three rheumatologists, two infectious disease doctors, and one hematologist at the cancer center prior to diagnosis by final rheumatologist.
Hindsight, my first flare was probably at age 20 when I ran fevers for four months and fatigue, and final diagnosis at UCLA at that time was some type of unknown virus that just went away so no further inquiries. I never experienced anything again until 2017, except unexpected weakness and swelling in left ankle periodically, severe tennis elbow in right arm periodically, and Reynaud’s syndrome. I had two bouts of pericarditis and one pleuritis that was assumed to be my asthma (I lived in area with high rate of Asthma due to air quality).
A rheumatologist finally diagnosed me after reviewing my complete medical history and running a few tests. The 10 months prior to diagnosis was frustrating. Going to doctor after doctor just to be told that they can’t find anything other than signs of severe inflammation in bloodwork can be very disheartening. All kept saying had to be autoimmune, but two rheumatologists said it wasn’t autoimmune and would send me to cancer or infectious disease doctors. The third rheumatologist was the charm! Luckily, I had a primary care internal medicine doctor that never gave up, he would do more research and send me to someone else, finally the right doctor!
For me, the largest problems has been repeated pericarditis. I get severe inflammation with any type of activity, no matter how minor; a walk around Sam’s Club can trigger it! Any type of extended activity, as in two or three stores in a day, then I put myself at risk of Pericarditis. I take Actemra injections weekly, Colchicine daily, and Prednisone on a tapered dose when I get pericarditis. As long as I pay attention to my body, don’t ignore the signs of fatigue by still pushing myself to be active, and don’t ignore the chest pressure at the beginning of flares, I am able to control it and stay off the steroids, or use limited tapered amounts. Unfortunately, I still suffer from daily fevers, none of the medications I have tried have stopped those. I have tried Kineret and Ilaris with no better results than the Actemra, and Methotrexate which gave me a severe allergic reaction called DRESS Syndrome. The Actemra and Colchicine keep the flares down to a minimum, but I still experience fevers, fatigue, inflammation, and pain.
It is difficult to adjust my lifestyle. I was forced to retire early due to this disease, which has been both a blessing and emotionally challenging. The blessing is my first grandchild arrived shortly after retiring and he has kept me mentally positive when I get down about my situation.
I am blessed that my family and friends have been very supportive of my condition. I have never felt the way many people with Stills disease say they do, that people don’t believe they are sick or think them lazy. I was very active prior to my illness and I think all my loved ones witnessed the change, so they are supportive. My husband witnesses my daily struggles with fevers and inflammation and is my strongest supporter!
I hope that more and more people become aware of Still’s disease, especially within the medical field. It is difficult to transition to new doctors (as I had to do when I relocated upon retirement to be closer to my kids). Many doctors know nothing about Still’s disease and that results in misunderstanding symptoms, missed diagnoses, etc. There is also such a limited amount of research in treatment options, approved medications, etc. A trip to the hospital is very scary for someone with Still’s if their doctor is not reachable, because it will be doubtful the ER docs will know what to do, and many of us end up worse by their treatments if we can’t get them to listen to us about Still’s Disease.
The more people who learn about Still’s Disease, and the more people advocate for that awareness, the more research will be conducted, and the more we will all learn about the disease. Be a voice!"
Staci's Story
Staci is diagnosed with Adult Onset Still's Disease.
"Hi, my name is Staci. I am 53 years old and live in the United States. I was diagnosed with Adult Onset Still's Disease, also known as AOSD, at the age of 45. This was after an almost year long battle of symptoms, several doctors, numerous doctor’s visits, and three hospital stays.
My story begins like this…On one cloudy, cool, rainy morning in March, my daughters and I went out to hit the local antique stores and resale shops for a girls day out. We had been out about 2 hours when one of them noticed that something was wrong and said, “ you don’t look like you feel well.” “ I stated I didn’t but let’s keep going because I was excited about our day. About half way through our next store, I said we are going to have to leave. I have a fever, chills and body aches. I went home and spent the rest of that day and Sunday in bed with just that low grade fever, chills, joint pain, headache and body aches. I was convinced that I had the flu, but little did I know that my life was about to change forever. Monday morning rolled around and I was fine-no symptoms. I went to work and everything was fine. A couple of weeks went by and my symptoms returned lasting a little longer this time around, but had disappeared by the time I could see my General Practitioner (GP). After several instances of this come and go flu as I called it, I decided to make an appointment with a doctor. When I went in for my visit, I explained my symptoms and how they had come and gone. I was feeling a bit tired at that time. Like the tired where you can’t get rested. She decided that my symptoms warranted some testing. So blood work was done. A couple of weeks later I went back in for the results only to find out that my inflammation levels were high, but everything else was rather normal. By this time, I was beginning to have a daily fatigue that I couldn’t seem to shake. She stated she had some ideas, but that she had to follow insurance protocol on what testing she could do. So again, we ran more bloodwork. A couple of weeks went by and I returned for my results: which again my inflammation levels were high, my RA factor was normal (which by the way Rheumatoid Arthritis is common in my family), however-my ANA came back positive. At this point, my fatigue had turned into exhaustion, I was continuing to have the sudden onset of my original symptoms: joint pain, low grade fever, body aches, but now I would have a sore throat to go along with the other symptoms. My GP explained how lots of people can have false positive ANA’s but that she decided to put me on medication to see if we could help lower my inflammation levels. She discussed Lupus, but I really was not presenting all the symptoms. She told me at this point not to give up on her. She has been my treating GP for many years and she knew me quite well. Even though at this point I was a little worried and frustrated, I trudged on. My symptoms continued to appear suddenly sometimes lasting for a couple of hours and sometimes a few days. I could be at work feeling fine talking to a co-worker and then in the next second feel awful to the point I would have to leave work and go home and go to bed. The two constant symptoms that I had was exhaustion and joint pain and they just continued to worsen. I had made several trips to the doctor over the course of the next few months. By September my spells became more frequent and my symptoms again had worsened. I made 3 trips in one week to the doctor-finally being admitted to the hospital with a 103-104 temp, nausea, vomiting, severe joint pain, severe chills(almost seizure like), extreme exhaustion. Again more blood work only for my ANA to be positive, my RA factor to be negative, my inflammation markers high. My medicine for my inflammation was changed and a follow-up appointment made. I was encouraged to start keeping a journal, logging each time I had a spell with the activity I was performing, what I had eaten for the day, and my symptoms with a scale system 1-5 on how bad they made me feel. Hoping to find some common factor that was bringing all of this on, I started keeping a journal. By the time, I went back in to see her-I had developed a rash. She discontinued my medicine as she thought I was allergic to it. A referral and an appointment with a Rheumatologist was made. My husband and I drove 3 hours to see this new doctor. I was so excited thinking there was a light at the end of the tunnel-finally some answers. I went to this new doctor with a journal in hand. Only to come away feeling very disappointed and defeated. My appointment went like this, how are you today?, what brings you here?, and a quick examination. She apparently had not read my records that my NP had forwarded her, she didn’t want to look at my journal. She didn’t want to run any tests. She looked at me as though I was making all of this up. She didn’t give me any answers as to what was happening with my body. She prescribed me two new medicines and scheduled me for a follow-up appointment. One medication was for inflammation and one for pain. I remember crying when we got to the car as I felt like I was never going to get any answers, and I was never going to get better. By this time, my symptoms had worsened to the point when I had an onset of symptoms-I could not be left alone. I couldn’t get out of the bed by myself and I had to have help walking as the joint pain and exhaustion was so extreme. I remember sitting on the side of our bed telling my husband as he was helping me to get up, because I couldn’t do it by myself, that I would never think about harming myself but that I certainly could see how someone could. I felt so helpless and alone, even though my husband, kids and sisters were helping me emotionally and physically. I felt like I was a burden as I couldn’t be left by myself when I had an onset of symptoms. I was exhausted and in so much pain. I just wanted to go to sleep and not wake up. And I never knew when the symptoms would decide to appear. Plans were put on hold, events with my grandkids, and lots of work was missed. I was beginning to feel as though I was going to lose my job which meant I would have no health insurance and less money. Looking back, I feel that the type of job I had at that time was probably why I didn’t lose my job. You see I worked for an Agency that helped the elderly and disabled get the services and help they needed. I was a good worker and didn’t miss work until I became sick. A few days of taking the new medications from the new doctor-I developed a horrible rash, vomiting, nausea, 104-105 temp, severe joint pain, headache, chills and exhaustion. I again ended up in the hospital. By this point, I was tired and done feeling bad. I felt like giving up. I had begun to do research on the Internet as I was not getting any answers from the doctors. The more research I did the more that led me to believe, I had Lupus. The more research I did about Lupus, the more the information led me to believe that I needed to go to a University Hospital. So after getting out of the hospital for the second time, I called my NP on the phone and explained the research I had done. I also told her how I felt about the Rheumatologist she had sent me too previously. I didn’t want to go back to her. I felt she really didn’t care about helping to get to the bottom of my illness and I was tired. I was tired of feeling sick and helpless. I was tired of missing family memories. I was tired of spending all my energy and money at the doctors for no answers. I then asked what she thought about sending me to a University Hospital. She too was stumped and didn’t know how else to help me as she too really thought we were moving in the right direction with the Rheumatologist she sent me too. She agreed. She was apologetic as she had not been able to help me. After doing her research she referred me to one of the local University Clinics. When the clinic called to make an appointment, I took the first appointment available. I couldn’t get in to see the doctor until the Day after Christmas and it was now the end of October. By this time, I was on another new medication and I had another trip to the hospital with the same symptoms that I had been hospitalized with previously. The holidays were approaching and I was feeling a bit stressed. I was excited and apprehensive about my appointment. However, I didn’t want to have a repeat of the last Rheumatologist appointment that I had. I had continued to do my own research and now had a list of questions myself to asked the doctor to go along with my journal. Christmas Day finally arrived and along with it so did the snow, sleet, and ice. My husband knew I was feeling anxious and scared so we cut our holiday visit with family short. We headed out for the 2 ½ hour drive for my appointment. He had decided that we needed to get a hotel room close to the University Clinic, so that I could make my appointment the next day. There was no way he was going to let the weather keep me from my appointment. We arrived at the clinic early for my appointment with my journal and questions in hand. My doctor was very interested in hearing my journey. He had read all the information that my GP had sent him, he took his time, he listened to me-my symptoms, my frustrations, and he examined me. He finally spoke the words-I really think that you have what is called Adult Onset Still's Disease but I can’t be certain. I would like to do some testing and monitor to you. I know it doesn’t sound like much, but after months of no answers I finally had a doctor who had some sort of answer. I felt a little relieved. He took me off all medications, done some tests, told me to keep my journal and made an appointment for me to return. He explained that AOSD is a very rare systemic inflammatory autoimmune disease, but did not go into a lot of detail. As soon as I got home, I got my computer out and started researching only to find there was not much information out there. I didn’t even get a hit on Wikipedia, WebMD, etc. I finally found the International Stills Foundation website. Only to find very limited information and a lot of medical terms that I had no clue what they meant. Now, I had become scared as there is a possibility that I have this rare disease that has no cure and I can’t find any information at all about it. I did join their blog and began to correspond with others that had the same symptoms as me, had the same emotions as me. Someone on the outside even though they were part of the inside that I could talk to and understood. That blog helped me tremendously. In February, almost a year after my symptoms began, I returned to the University Clinic and received my official diagnosis of AOSD and medication to manage my disease. I have been living with Stills now for 8 years. My life has changed, as has the awareness and information about Stills. You now can search the Internet and find information about Stills on Wikipedia, WebMD, etc. With the help of my doctor, my medication, my self awareness, my family and my discipline, I have learned how to manage my disease. My biggest accomplishment was learning to lean on my support system and to say no. Its very important to know your body and it’s limits. As stress can bring on what I now know is called Flares. Educate yourself to be able to ask questions. Don’t be afraid to speak up for yourself when you have suggestions about your treatment-our doctors are very busy. Yes I know, what you are thinking-they are your doctor and they should know when you need assistance, but they are Human too. So, you have to keep them informed of your disease and the changes that may be taking place. You know your body best. Remember not everyone has the same symptoms-our bodies are all different and react differently. Be prepared-Be flexible-Be sensible. Make decisions that help you to stay well. And most importantly educate others. The more people who know about Stills-the more research that will be done, the more understanding there will be, the more information that will be available for us and those just being diagnosed, and the better we will be able to manage our disease. Please if you have a family member, a friend or co-worker with Stills, be supportive of them. Don’t give up on them and encourage them not to give up on themselves. Advocate for them and for Stills. If it wasn’t for my husband, kids, sisters and a good friend, I would have given up before I received my diagnosis and the correct medicine. We need the support. #mystillsstory #iamadragonslayer"
Hannah's Story
Hannah is diagnosed with Adult Onset Still's Disease.
"On my 18th birthday, I began running a fever. After my birthday, I continued running a fever every night. My primary care physician ran multiple lab work and nothing really came back. I was sent to see an Infectious Disease Specialist, who found nothing. For about one year, that was the only symptom I had until my finger and top of my hand hurt. After wearing a brace, having multiple injections, taking anti-inflammatories, and having an MRI that showed nothing, the orthopedic decided to test my SED rate and RH factor which both came back high.
I was referred to a rheumatologist here in Evansville. An ultrasound was ordered to check for joint swelling in my hand. The ultrasound showed no joint swelling as did the physical exam of my joints in the office. She provided me with the probable diagnosis of Rheumatoid Arthritis that just hadn’t manifested all the way. I was started on a very low dose of Plaquenil. It didn’t help much but she told me until I started showing joint swelling, she wasn’t going to change my medicine. She told me that if I had seen her 6 months after the fevers started, she would have sent me to see an Oncologist to be screen for leukemia. It had been two years of having fevers but after talking with my parents, we asked to be referred to see an oncologist to make sure we were able to rule things out!
After seeing the oncologist multiple times, he gave me the all clear from him. He suggested that I either travel down to Vanderbilt or IU to have a second opinion. I shared that information with my rheumatologist and she told me that I didn’t have an autoimmune disease and that doctors at those facilities would be able to tell me anything. We demanded she send a referral down to Vanderbilt Rheumatology which she reluctantly did.
I had an appointment at Vanderbilt in March but due to COVID-19 it was canceled and rescheduled for June. In June, I was given the diagnosis of Still’s Disease. I felt so relieved to have a diagnosis that made more sense for the symptoms that I had. The symptoms that I had and still have are daily fevers with red cheeks that are hot to touch, fatigue, and slight joint pain but no join swelling. The doctor kept me on my Plaquenil but also started me on Methotrexate and Folic Acid! Those medications have helped tremendously! I don’t hurt as much as I did before. There are days that I hurt all day but that’s going to happen! Fevers are still a daily thing but I’m honestly used to them since it’s been almost 4 years!
Before I was diagnosed, I felt very frustrated because I knew the diagnosis of Rheumatoid Arthritis wasn’t the correct one because of the symptoms that I had. I figured that I wasn't going to have a diagnosis that made sense for a long time or ever. But after I was diagnosed, I was so relieved because this diagnosis made so much more sense.
Still’s Disease has impacted my life in many ways! I have had to cancel multiple times on plans because of the pain I was in. I feel as sometimes that I haven’t gotten to experience the full college experience because of my Still’s and the pain/fatigue that comes with it. I’ve spent numerous hours in doctor offices, traveling for appointments, waiting for lab work, etc. On the other hand, Still’s disease has allowed me to learn to stand up and advocate for myself. I feel like I have grown as an individual since all of this began almost 4 years ago.
I have found finding a Still’s Disease support group helps a lot! It’s so good to be able to talk to others that have similar conditions and symptoms as you! Don’t be afraid to ask/send your doctor a message with any questions or concerns about it!
Bringing awareness to Still’s disease is important so other people know what it is exactly and also have hope that a correct diagnosis is out there for them! "